PPI Kidney Damage: What You Need to Know About Long-Term Use Risks
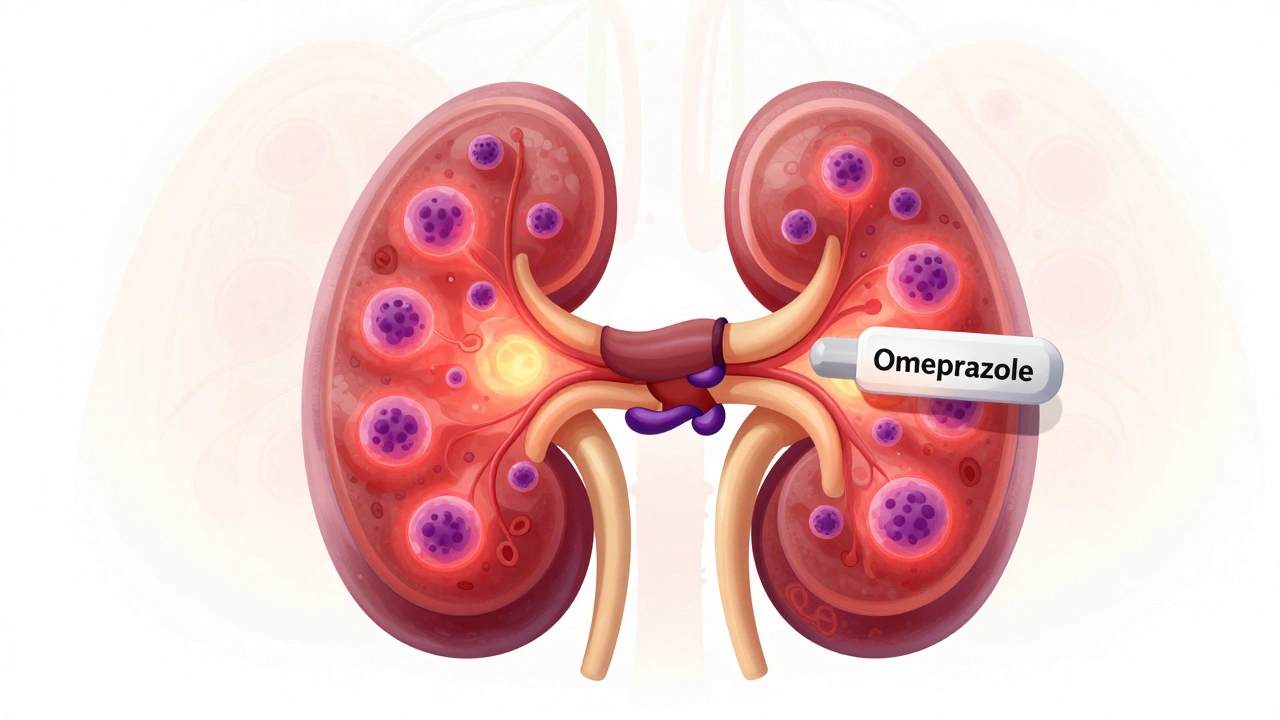
When you take a proton pump inhibitor, a class of drugs used to reduce stomach acid, commonly prescribed for heartburn, GERD, and ulcers. Also known as PPIs, these medications include omeprazole, esomeprazole, and lansoprazole—drugs millions rely on daily for relief. But behind the quick relief is a quiet risk: PPI kidney damage, a growing concern linked to long-term use, especially in people who take these drugs for years without medical oversight. It’s not a sudden crisis—it’s a slow, silent decline in kidney function that often goes unnoticed until it’s advanced.
Studies show that people using PPIs for more than a year have a higher chance of developing chronic kidney disease, a condition where kidneys lose their ability to filter waste over time. This isn’t just theory—research published in JAMA Internal Medicine found that long-term PPI users were up to 20% more likely to develop kidney problems compared to those using other acid reducers like H2 blockers. The damage often shows up as interstitial nephritis, an inflammation of kidney tissue, or as a drop in estimated glomerular filtration rate (eGFR). It’s not just older adults at risk. Even healthy people in their 30s and 40s who take PPIs daily for years can see changes in their kidney labs.
Why does this happen? PPIs reduce acid to help the stomach, but they also affect how the kidneys handle minerals and electrolytes. Over time, this can trigger inflammation, scarring, and reduced blood flow to kidney tissues. The risk goes up if you’re also taking NSAIDs, diuretics, or have high blood pressure or diabetes. And here’s the catch: many people don’t realize they’re on PPIs long-term. They start for a short course, feel better, then keep taking them because "it’s just an antacid." But these aren’t harmless supplements—they’re powerful drugs with real side effects.
If you’ve been on a PPI for more than six months, ask your doctor if you still need it. Some people can switch to lifestyle changes—eating smaller meals, avoiding late-night snacks, cutting back on caffeine and alcohol—or try H2 blockers like famotidine, which carry less kidney risk. Others may need to taper off slowly to avoid rebound acid. Your kidneys won’t warn you until it’s too late, but your bloodwork can. A simple creatinine test and eGFR check can catch early signs of trouble.
Below, you’ll find real-world posts from people who’ve dealt with medication side effects, kidney health concerns, and how to spot problems before they escalate. From how to monitor your meds to understanding what happens when you take drugs long-term, these articles give you the tools to ask the right questions—and protect your body while you manage your symptoms.