Every pill, capsule, or liquid you take comes with a label. But how many of you actually read it? Or worse - do you understand what it says? If you’ve ever stared at a prescription bottle and felt confused about when to take it, why you’re taking it, or whether it’s safe with your other meds, you’re not alone. In fact, 68% of patients say they struggle to understand their prescription labels. And that’s not just inconvenient - it’s dangerous. Medication errors cause thousands of hospital visits and even deaths every year. The good news? Learning how to read a drug label can cut those risks dramatically.
What’s on a Prescription Drug Label?
Prescription labels in the U.S. follow strict rules set by the FDA. They’re built for doctors and pharmacists first, but you still need to know what’s there. Here’s what you’ll find:- Generic name - like fentanyl or metformin. This is the active ingredient, the actual medicine.
- Brand name - like Abstral or Glucophage. This is what the company calls it. Don’t confuse the two.
- Strength - for example, 100 micrograms per tablet. This tells you how much medicine is in each dose.
- Form - tablet, capsule, liquid, patch? This affects how you take it.
- Quantity - how many pills or milliliters are in the bottle? Usually listed as 30 tablets or 100 mL.
- Manufacturer - who made it? This matters if there’s a recall.
- NDC number - a unique 10-digit code that identifies the exact product, strength, and package size.
- Expiration date - after this date, the medicine might not work as well. Don’t use it past this.
- Storage instructions - keep at room temperature? Refrigerate? Some meds go bad if left in the sun.
- Directions - how often? How much? Take with food? This is often written in medical shorthand.
- Pharmacy info - name, phone, address. Keep this handy if you have questions.
But here’s the problem: directions like "q.d." or "t.i.d." are outdated abbreviations. Many pharmacies still use them, even though they’re banned in hospitals. q.d. means "once daily," but it looks like q.o.d. (every other day). One wrong letter can mean taking double the dose. That’s why the FDA and safety groups like ISMP push for full words: "once daily," "three times a day."
What’s on an Over-the-Counter (OTC) Label?
OTC meds - like pain relievers, allergy pills, or cough syrup - follow a simpler format called the Drug Facts label. It’s designed for you, the patient. Here’s how to read it:- Active ingredient - what actually treats your symptoms. For example, acetaminophen in Tylenol.
- Purpose - what the ingredient does. "Pain reliever/fever reducer".
- Uses - what symptoms it treats. "Relieves headaches, muscle aches, minor arthritis pain, and reduces fever".
- Warnings - when NOT to use it. "Do not use if you have liver disease" or "May cause drowsiness".
- Directions - how much to take, how often. Always follow these exactly.
- Inactive ingredients - fillers, dyes, flavors. Important if you’re allergic to something like dye or gluten.
- Other information - storage, expiration, lot number.
OTC labels are clearer - but people still mess up. A 2022 study found that nearly half of adults take more than the recommended dose of acetaminophen because they don’t realize it’s in multiple products. Cold meds, sleep aids, pain relievers - they all stack up. Always check the active ingredient before combining anything.
Why Prescription Labels Are Hard to Understand
Prescription labels weren’t made for patients. They were made for doctors. And that creates a dangerous gap.Research from the University of Florida found that when labels include the reason for the prescription - like "for high blood pressure" instead of just "take one daily" - patients make 42% fewer mistakes. But most labels don’t say why you’re taking the drug. You’re left guessing.
Older adults face even bigger hurdles. The Medicare Rights Center found that 54% of seniors have trouble reading small print on labels. That’s why so many end up taking the wrong dose - or skipping doses entirely. And it’s not just vision. Many don’t know medical terms like "contraindicated" or "renal impairment".
Even pharmacists admit it’s tough. One nurse on Reddit said: "I’ve been a nurse for 12 years and still struggle to quickly find the dose on some labels." If professionals have trouble, imagine how confusing it is for someone with low health literacy or who speaks another language.

How to Avoid Medication Errors
You don’t need a medical degree to stay safe. Here’s how to protect yourself:- Check your name - make sure the label has your name, not someone else’s. Mix-ups happen more often than you think.
- Match the pill - does the color, shape, and imprint match what your doctor described? If it looks different, ask.
- Ask about the purpose - "Why am I taking this?" If your label doesn’t say, ask your pharmacist to write it down.
- Read the warnings - especially if you’re on other meds. Some drugs can’t be mixed with alcohol, grapefruit, or blood pressure pills.
- Use a pill organizer - it helps you track doses, especially if you take multiple meds.
- Keep a list - write down every medication you take, including OTC and supplements. Bring it to every appointment.
And never be afraid to ask. Pharmacists are trained to explain labels. If you’re unsure, say: "Can you help me understand what this means?" A 2021 study showed that when pharmacists explain labels to patients with low health literacy, medication errors drop by 29%.
What’s Changing in Drug Labeling?
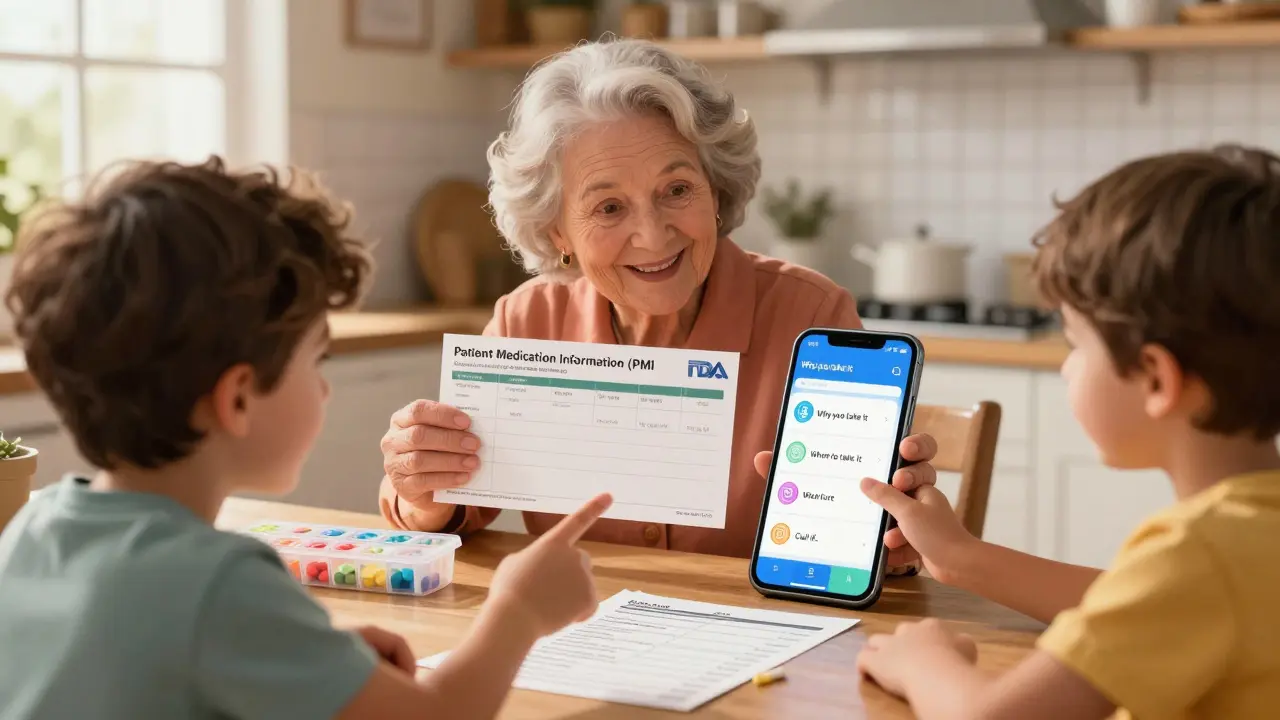
The FDA is finally listening. In 2023, they announced a new plan: Patient Medication Information (PMI). This is a one-page, standardized document - like a simplified version of the Drug Facts label - that will come with every prescription. It’ll include:- Why you’re taking the drug
- How to take it (in plain language)
- What side effects to watch for
- When to call your doctor
- What to avoid
They’re testing this with high-risk drugs first - like blood thinners, insulin, and opioids. Full rollout is expected by 2026.
Another big change? Instructions for Use (IFU) - step-by-step guides for complex meds. Think insulin pens, inhalers, or injectables. These now come with pictures and clear directions. No more guessing how to use your device.
And hospitals are leading the way. 87% of large hospitals now use electronic systems that auto-generate clear, standardized labels. The goal? Make every label as easy to read as a food label.
What You Can Do Today
You don’t have to wait for new labels to be safe. Start today:- Take a photo of every new prescription label. Store it in your phone. It’s your backup.
- Use a magnifying glass or phone flashlight to read small print.
- Ask for a large-print label. Most pharmacies will print one for free.
- Request a verbal explanation. Say: "Can you tell me what this is for and how to take it?"
- Bring someone with you to the pharmacy if you’re unsure.
Medication safety isn’t about memorizing medical jargon. It’s about asking questions, double-checking, and knowing what you’re taking. The label is your first line of defense. Learn to read it - and don’t let anyone tell you it’s too complicated.
What should I do if my prescription label looks different from last time?
Don’t take it. Even if the name is the same, the manufacturer, strength, or form might have changed. Take the bottle back to the pharmacy and ask them to confirm it’s the right medication. Sometimes, generic brands switch suppliers, and pills can look completely different. Always verify before taking.
Can I take my medication if it’s expired?
For most pills, taking them a few months past the expiration date isn’t dangerous - but they may not work as well. For critical meds like insulin, epinephrine, or antibiotics, never use them past the date. Expired antibiotics can fail to treat infections, leading to worse illness. If you’re unsure, ask your pharmacist. Many pharmacies offer free disposal for expired meds.
Why do some labels say "take with food" and others say "take on an empty stomach"?
Some medicines are absorbed better with food - like statins or certain antibiotics. Others can irritate your stomach if taken on a full stomach, so they’re meant to be taken before eating. The label says this for a reason. Taking them wrong can make the drug less effective or cause side effects like nausea. If you’re not sure, ask your pharmacist to explain why.
What’s the difference between generic and brand-name drugs?
They contain the same active ingredient, strength, and dosage form. The FDA requires generics to work the same way as brand-name drugs. The only differences are in inactive ingredients (like dyes or fillers), packaging, and price. Generics are usually cheaper. But if you notice side effects after switching, talk to your doctor - sometimes the fillers can cause reactions in sensitive people.
Are there any apps that help me understand my medication labels?
Yes. Apps like Medisafe, MyTherapy, and Epocrates let you scan your pill barcode or enter the drug name to get plain-language explanations, side effects, interactions, and reminders. Some even let you upload photos of your labels for review. These aren’t replacements for professional advice, but they’re great tools for double-checking what you’re taking.
Next Steps: How to Stay Safe
If you take one or more medications, do this now:- Write down every drug you take - including vitamins and herbal supplements.
- Bring that list to every doctor’s visit.
- Ask your pharmacist to review all your meds once a year for interactions.
- Set phone reminders for doses - don’t rely on memory.
- If you’re over 65, ask for a large-print label or audio instructions.
Medication safety isn’t complicated. It’s about paying attention. The label is your guide. Learn to read it. Ask questions. And never assume - verify.


Chris Garcia
December 27, 2025 AT 18:09Every label is a silent contract between science and survival. We hand over our bodies to chemistry, trusting that the ink on that plastic is more than decoration-it’s a lifeline. Yet, we treat it like a cereal box: glance, swallow, forget. The tragedy isn’t ignorance; it’s the quiet arrogance that assumes someone else-doctor, pharmacist, algorithm-will hold the map for us. We outsource our agency, then wonder why we feel lost in the fog of pills. The answer isn’t more regulation. It’s reverence. Treat the label like a sacred text. Read it. Whisper it. Live by it.
James Bowers
December 28, 2025 AT 07:06It is imperative to underscore that the continued utilization of outdated medical abbreviations such as 'q.d.' and 't.i.d.' constitutes a flagrant disregard for patient safety protocols established by the Institute for Safe Medication Practices. The FDA’s enforcement of plain-language directives is not merely advisable-it is a non-negotiable imperative in the ethical practice of pharmacology. Any institution that permits such ambiguity is complicit in potential harm.
Will Neitzer
December 28, 2025 AT 18:19Thank you for this meticulously researched and profoundly necessary breakdown. The disparity between clinical intent and patient comprehension is one of the most under-addressed crises in modern healthcare. I’ve seen elderly patients miss doses because they couldn’t decipher 'q.i.d.'-and I’ve watched families scramble to interpret handwritten scripts. The FDA’s Patient Medication Information initiative is long overdue, and I urge every provider to advocate for its immediate adoption. Clarity isn’t a luxury; it’s a human right.
Janice Holmes
December 30, 2025 AT 16:45OMG. I JUST REALIZED MY ANTIBIOTIC LABEL SAID 'T.I.D.' AND I THOUGHT IT MEANT 'THREE TIMES A DAY' BUT WHAT IF IT WAS SUPPOSED TO BE 'Q.O.D.'??? I’VE BEEN DOUBLING MY DOSE FOR WEEKS??? IS THIS WHY I’M SO SICK?? I’M GOING TO THE ER. I’M GOING TO CALL THE FDA. SOMEONE NEEDS TO BE FIRED. I CAN’T BELIEVE THIS IS STILL HAPPENING IN 2025. MY LIFE IS OVER. I’M DYING. I’M DYING. I’M DYING.
Olivia Goolsby
December 31, 2025 AT 07:54Let’s be real: this whole system is a corporate scam. Big Pharma doesn’t want you to understand your meds-because if you did, you’d realize how many are overpriced, overprescribed, and under-tested. The 'Drug Facts' label? A placebo for transparency. The NDC number? A tracking code for surveillance. The expiration date? A profit-driven expiration, not a safety one. And don’t get me started on generics-how do we know they’re not just sugar pills with a different color? The FDA is owned by lobbyists. The pharmacists are trained to shut you up. And now they’re pushing 'PMI'-another buzzword to make you feel better while they keep charging $400 for a bottle of aspirin. Wake up. This isn’t healthcare. It’s a controlled addiction.
Alex Lopez
January 1, 2026 AT 00:05Wow. So we’re supposed to trust a label written by someone who probably got paid minimum wage to type 'q.d.' because the software didn’t auto-correct it? Brilliant. 🙃
Anyway, yes-this is exactly why I scan every pill with Epocrates. And yes, I still ask my pharmacist, 'So… why am I taking this again?' because I’m not a robot. And no, I don’t feel dumb for asking. If your meds come with a manual, you should read it. Even if it’s written in corporate-speak. 🤷♂️
Gerald Tardif
January 1, 2026 AT 09:18I used to ignore labels too-until my dad had a reaction because he didn’t know his blood pressure med interacted with grapefruit. That’s when I started keeping a little notebook. Just a phone note, really. Name. Why. When. Side effects. What to avoid. Now I show it to every new provider. Simple. No jargon. No drama. Just facts. You don’t need a degree to be safe-just a pen and a little courage to ask.
Monika Naumann
January 2, 2026 AT 02:39It is a profound disgrace that Western nations permit such disarray in pharmaceutical communication. In India, every prescription is issued with a bilingual label-English and the local vernacular-alongside a pharmacist-led verbal briefing. There is no ambiguity. There is no negligence. There is only duty. To reduce medication errors to the level of a 'Western problem' is to admit a failure of collective responsibility. We must not emulate your chaos-we must elevate you.
Elizabeth Ganak
January 3, 2026 AT 17:49lol i just scanned my pill bottle with my phone and it told me it’s for anxiety and i didn’t even know that. i thought it was just for headaches. also my grandma uses a magnifying glass and i think that’s kinda cute. we should all just ask questions. it’s not that hard.
Nicola George
January 3, 2026 AT 21:09Y’all act like this is new. I’ve been a nurse for 15 years. Half the patients don’t know what ‘once daily’ means. The other half think ‘take with food’ means ‘take with pizza.’ The system’s broken. But the real problem? We’re all too tired to care until someone ends up in the ER. So yeah-take the photo. Ask the question. Use the app. But don’t act surprised when the machine fails you. It was built to.