Disseminated Intravascular Coagulation: Causes, Risks, and What You Need to Know
When your blood starts clotting all over the place — then suddenly won’t clot at all — you’re looking at disseminated intravascular coagulation, a life-threatening condition where the body’s clotting system goes out of control. Also known as DIC, it doesn’t happen on its own. It’s always triggered by something else, like severe infection, trauma, or cancer. This isn’t just a lab finding. It’s a medical emergency that can turn a patient from stable to critical in hours.
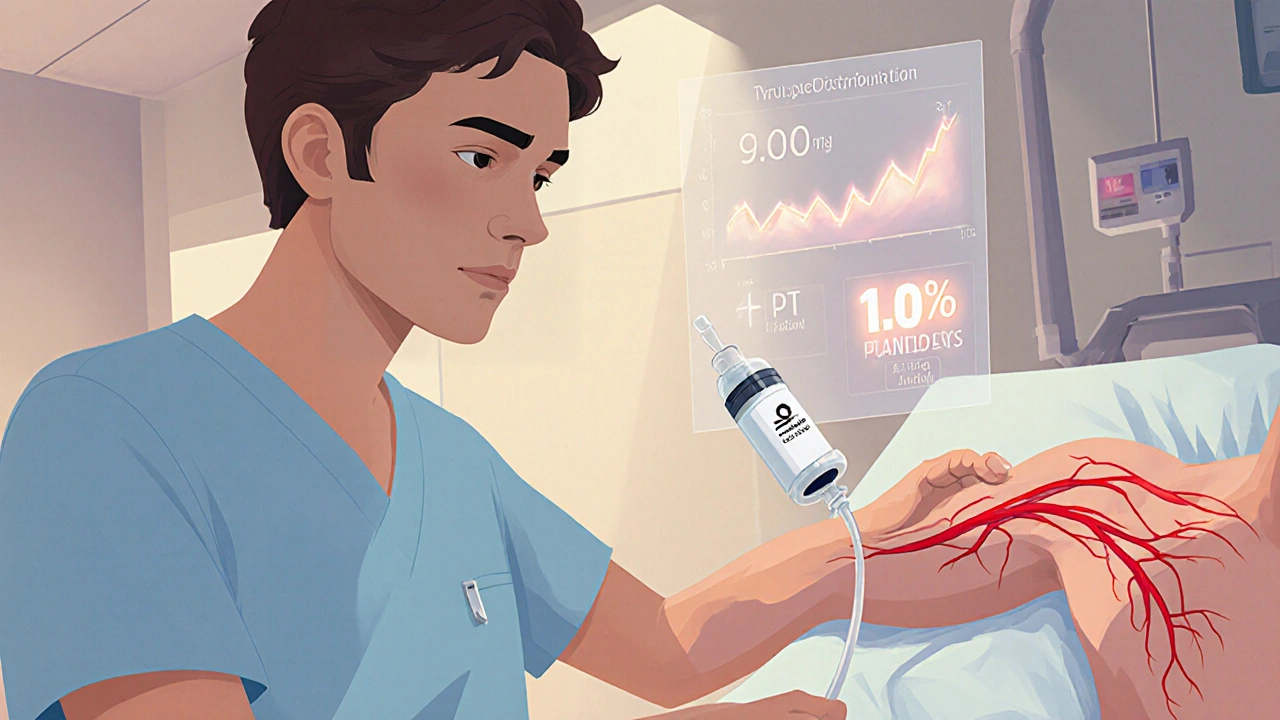
Think of your blood clotting system like a fire alarm. Normally, it goes off only when there’s a real fire — say, a cut or injury. In disseminated intravascular coagulation, the alarm goes off nonstop, even when there’s no fire. Clots form in tiny vessels all over the body — in the kidneys, brain, lungs. Those clots block blood flow, damage organs, and use up your clotting resources. Once those resources are gone, you start bleeding uncontrollably — from IV sites, gums, even internally. That’s why DIC patients often show both clots and bleeding at the same time.
What causes this mess? Common triggers include sepsis (especially from bacteria like E. coli or meningococcus), major trauma like car crashes, complications during pregnancy like placental abruption, and certain cancers — particularly leukemia or advanced solid tumors. sepsis, a systemic infection that overwhelms the body is the #1 cause. If you’re in the hospital with a bad infection and your labs show low platelets and rising fibrin degradation products, DIC is likely on the table.
It’s not something you can treat with a simple pill. Managing disseminated intravascular coagulation, requires fixing the root problem while supporting the body’s broken clotting system. That means antibiotics for infection, surgery for trauma, chemo for cancer — and sometimes blood products like platelets or fresh frozen plasma to replace what’s been used up. But giving clotting factors blindly can make things worse. That’s why doctors rely on lab tests: platelet count, fibrinogen, PT/INR, D-dimer. These aren’t just numbers. They’re clues to whether the body is making more clots or bleeding out.
You won’t find a cure in a supplement or herbal remedy. This is hospital-level care. But understanding how it works helps you ask the right questions if you or someone you love is at risk. The posts below cover related topics — from how infections trigger systemic responses, to how bleeding disorders are diagnosed, to the drugs that can affect clotting. None of them treat DIC directly. But together, they give you the context to understand why it happens, how it’s managed, and what makes it so dangerous. What you’ll see here isn’t just theory. It’s the real-world science behind the headlines — and the practical details that matter when lives are on the line.