When you're taking an SSRI antidepressant like sertraline or escitalopram, you might assume you're safe as long as you stick to your prescription. But what if you also take tramadol for back pain, or St. John’s wort for low mood, or even linezolid for a stubborn infection? These aren't rare combinations - they happen every day. And when they do, they can push your brain’s serotonin levels into dangerous territory. This isn't a theoretical risk. It's called serotonin syndrome, and it can turn a routine medication routine into a medical emergency.
What Exactly Is Serotonin Syndrome?
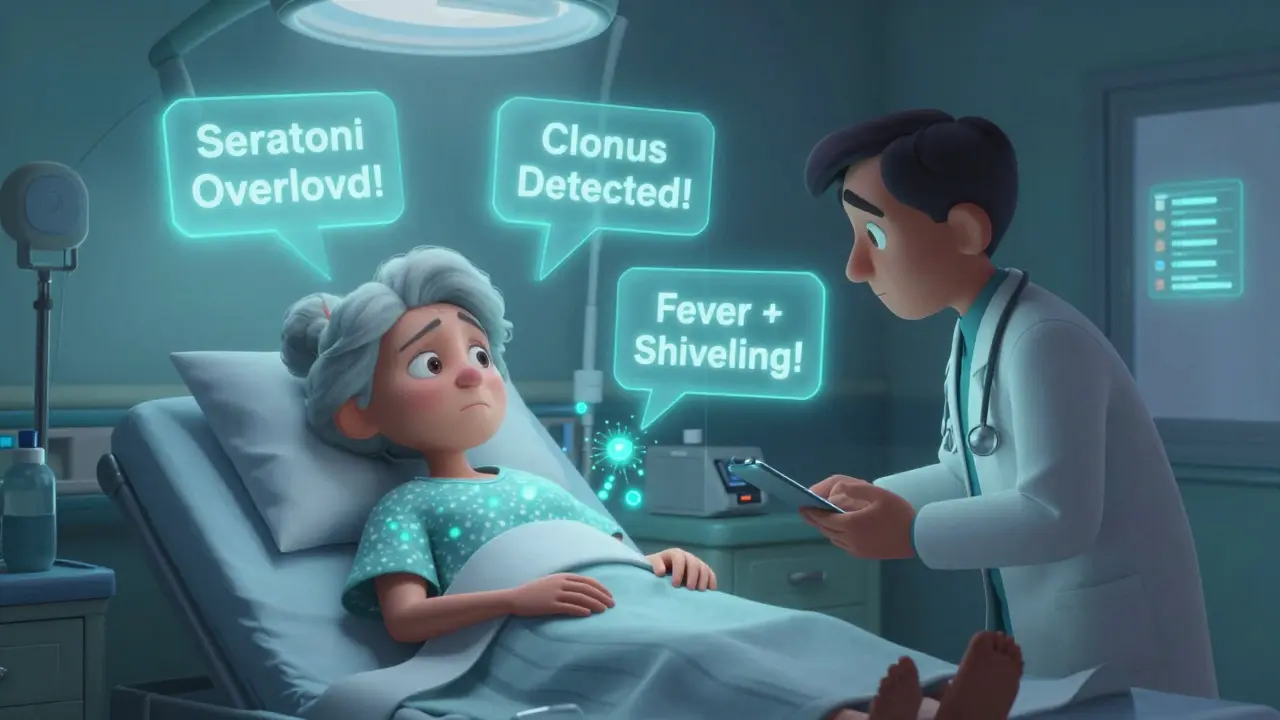
Serotonin syndrome isn't just "feeling a little off." It's a real, potentially deadly condition caused by too much serotonin activity in your nervous system. Think of serotonin as a chemical messenger. SSRIs work by blocking its reabsorption, so more stays around to improve mood. But when other drugs add even more serotonin - or stop it from being broken down - the system gets overloaded. Symptoms don't sneak up slowly. They hit hard and fast: muscle rigidity, high fever, rapid heartbeat, confusion, tremors, or uncontrollable shivering. In severe cases, it leads to seizures, organ failure, or death.
The Hunter Criteria, used by doctors today, are the gold standard for diagnosis. You don’t need every symptom. Just one key sign - like spontaneous clonus (involuntary muscle contractions) plus fever or agitation - is enough to raise serious alarms. And here’s the catch: many cases are missed because symptoms look like the flu, a panic attack, or even drug withdrawal.
The Biggest Culprits: Which Drugs Raise the Risk?
Not all drug combinations are equal. Some are mild, others are ticking time bombs. Let’s break it down by risk level.
High-risk combinations: These are the ones you absolutely must avoid unless there’s no other option.
- MAOIs (like phenelzine or selegiline): Combining an SSRI with an MAOI is like pouring gasoline on a fire. The FDA and global health agencies call this contraindicated. The mortality rate when this happens is 30-50%. Even a two-week gap between stopping one and starting the other isn’t always enough - especially with fluoxetine, which lingers in your system for weeks.
- Linezolid (antibiotic): This drug, used for tough infections like MRSA, blocks serotonin breakdown. A 2022 JAMA study found patients over 65 on SSRIs who took linezolid had nearly triple the risk of serotonin syndrome. It’s rare, but deadly when it hits.
- Tramadol, pethidine, dextromethorphan: These aren’t your typical opioids. Tramadol, for example, doesn’t just relieve pain - it also boosts serotonin. A 2023 study found this combo increases serotonin syndrome risk by 4.7 times. Patients on Reddit have described hospitalization after just one dose of tramadol with sertraline.
Medium-risk combinations: These need caution and monitoring.
- SNRIs (like venlafaxine or duloxetine): Combining two antidepressants that both raise serotonin - even if they’re different classes - increases risk by over 3 times. The FDA added a black box warning for this in 2006.
- Methadone and fentanyl: These opioids have a dual effect. They bind to opioid receptors, but also interfere with serotonin clearance. Risk jumps by 2.1 times.
Low-risk combinations: These are generally safe.
- Morphine, codeine, oxycodone, buprenorphine: These opioids don’t significantly affect serotonin. Studies show no meaningful increase in risk. If you need pain relief while on an SSRI, these are the safer choices.
Other Hidden Risks You Might Not Know About
It’s not just prescription drugs. Some supplements and over-the-counter meds sneak under the radar.
- St. John’s wort: This herbal remedy for mild depression is a potent serotonin booster. One user on Drugs.com described developing confusion and shivering after just three days of combining it with Prozac. ER doctors confirmed early serotonin syndrome.
- Tryptophan and 5-HTP: Sold as sleep or mood aids, these are direct serotonin precursors. They shouldn’t be near SSRIs.
- Buspirone (anxiety med): Often prescribed with SSRIs, but it adds to serotonin levels. Use only under close supervision.
- Lithium: Used for bipolar disorder, it can amplify SSRI effects. The combination requires frequent blood monitoring.
Who’s Most at Risk?
It’s not just about what you take - it’s who you are.
- Elderly patients: Over 21% of Americans 60+ take SSRIs. Nearly 18% also take opioids for chronic pain. On average, Americans over 65 take five or more medications daily. That’s a recipe for dangerous overlaps.
- People on multiple antidepressants: Switching from one SSRI to another? Stopping an SNRI while starting an SSRI? If you don’t wait long enough - especially with fluoxetine - you’re playing Russian roulette with your nervous system.
- People with genetic differences: A 2023 study from UCSF found that people who are CYP2D6 poor metabolizers (about 7% of Caucasians) break down tramadol slowly. This doubles their risk of serotonin syndrome when combined with SSRIs.
What Should You Do?
Don’t panic. But do take action.
- Know your meds. Make a list - all of them. Prescription, OTC, supplements. Bring it to every appointment.
- Ask your doctor: "Could this interact with my SSRI?" Don’t assume they know. Many prescribers don’t realize tramadol is a serotonin booster.
- Watch for the 5 S’s: As the Cleveland Clinic advises: Shivering, Sweating, Stiffness, Seizures (rare), and Sudden confusion. If you notice even two of these after starting a new drug, get help immediately.
- Don’t stop your SSRI suddenly. Withdrawal can mimic serotonin syndrome. Always taper under supervision.
- Use a pharmacist. A 2023 study showed pharmacist-led reviews cut serotonin syndrome events by 47%. Pharmacists are trained to catch these interactions.

What’s Changing in 2026?
The system is finally catching up. The FDA now requires all e-prescribing systems to show mandatory alerts when high-risk combinations are prescribed. By 2026, a blood test called SerotoninQuant may become available - the first objective diagnostic tool. The CDC’s 2024 opioid guidelines now explicitly say: avoid tramadol, dextromethorphan, and pethidine in SSRI users. Instead, use morphine or oxycodone.
But the core message hasn’t changed: SSRIs are safe - until they aren’t. The danger isn’t the drug itself. It’s the invisible combinations. The ones you don’t think about. The ones you don’t tell your doctor about.
Can serotonin syndrome happen with just one SSRI?
Rarely. Most cases occur when SSRIs are combined with other serotonergic drugs. However, overdose of a single SSRI - especially with slow-metabolizing ones like fluoxetine - can trigger serotonin syndrome. It’s uncommon but possible.
How long should I wait between stopping an SSRI and starting an MAOI?
At least two weeks. But if you were taking fluoxetine (Prozac), wait five weeks. Its active metabolite stays in your system much longer than other SSRIs. Skipping this step can be fatal.
Is it safe to take ibuprofen or acetaminophen with an SSRI?
Yes. Neither ibuprofen nor acetaminophen affects serotonin levels. They’re safe to use with SSRIs for pain or fever. Avoid combination cold medicines that contain dextromethorphan or tryptophan.
Can serotonin syndrome be diagnosed with a blood test?
Not yet in routine practice. Diagnosis is based on symptoms and history. But a new test called SerotoninQuant is in phase 3 trials and may be available by 2026. It measures serotonin levels directly, which could revolutionize diagnosis.
What should I do if I think I have serotonin syndrome?
Seek emergency care immediately. Call 911 or go to the nearest ER. Do not wait. Symptoms can worsen rapidly. Tell the medical team you’re taking an SSRI and any other drugs or supplements. Early treatment - stopping the drugs and giving supportive care - can be lifesaving.
Are there any safe alternatives to tramadol for pain if I’m on an SSRI?
Yes. Morphine, oxycodone, and buprenorphine are considered low-risk for serotonin syndrome. Talk to your doctor about switching. Non-drug options like physical therapy, acupuncture, or nerve blocks may also help reduce reliance on opioids entirely.
Why don’t more doctors warn patients about this?
Many don’t realize how common the interactions are. A 2022 study found over 60% of SSRI-opioid combinations were prescribed without documented risk assessment. Patient education is still inconsistent. That’s why it’s critical to ask questions yourself - and keep a full medication list.
Final Takeaway
SSRIs changed how we treat depression. But they’re not risk-free. The real danger isn’t the pill in your medicine cabinet - it’s the unknown combo you didn’t think to ask about. Whether it’s a new painkiller, an herbal supplement, or a course of antibiotics, every new medication needs to be checked against your SSRI. Don’t wait for symptoms. Don’t assume it’s fine. Talk to your pharmacist. Write it down. Ask twice. Because when it comes to serotonin syndrome, ignorance isn’t just dangerous - it’s deadly.


Randy Harkins
February 8, 2026 AT 21:29Just wanted to say thank you for writing this. I’ve been on sertraline for 5 years and just started tramadol for a herniated disc last month. I had no idea there was even a risk. I’m going to my pharmacist tomorrow to get it checked. Seriously, this could’ve gone sideways. You’re doing important work.
Elan Ricarte
February 10, 2026 AT 14:10Oh sweet mother of Christ, another one of these "I’m a doctor in my head" posts. You think because you listed 17 drugs you’re some kind of serotonin oracle? Newsflash: most people don’t even know what an SSRI stands for. And yet you’re out here acting like you’re the first person to ever warn about tramadol + Zoloft? Bro. Just… bro. I’ve seen this exact post in 3 different subreddits. Copy-paste much?
Marie Fontaine
February 11, 2026 AT 16:37YESSS this is so needed!! I took St. John’s wort with my Lexapro for 3 weeks and felt like I was having a panic attack + fever dream. Went to the ER and they were like "ohhh you’re one of those" 😅 I’m so glad you included supplements - so many people think "natural" = safe. Nope. Natural can kill you too. 💪
Lyle Whyatt
February 11, 2026 AT 20:55Let me tell you something - I’m an Aussie GP with 18 years in primary care, and I’ve seen this exact scenario play out three times in the last year alone. One 72-year-old woman on sertraline, linezolid for a UTI, and a daily dose of 5-HTP because "it helps her sleep." She developed clonus, hyperthermia, and a heart rate of 152. Took 48 hours to stabilize. The worst part? She didn’t even tell her doctor about the supplement. We’re not talking about rare outliers here. This is a systemic failure of communication. Every single patient on an SSRI needs a mandatory med review before any new prescription or OTC is added. Pharmacists are the unsung heroes here. We need to stop treating them like pill dispensers and start treating them as clinical partners. It’s not just about avoiding serotonin syndrome - it’s about building a culture of safety, not just compliance.
Tatiana Barbosa
February 12, 2026 AT 04:52As someone who’s been on SSRIs + lithium for bipolar II, I’m screaming at my screen. YES. The CYP2D6 poor metabolizer thing is real. My genetic test flagged me last year. My psych said "don’t touch tramadol, dextro, or even some OTC cold meds." I didn’t even know my body processed meds differently. This post is a godsend. Also - pharmacist reviews cut events by 47%? That’s insane. My pharmacy does free med reviews. I’m going tomorrow. Thank you for the clarity.
Ken Cooper
February 12, 2026 AT 12:43wait so if i’m on citalopram and i take a cold med with dextromethorphan… is that bad? i’ve done it like 3 times… also what about melatonin? is that safe? and i use ibuprofen for headaches all the time… is that ok? lol i’m so confused now
MANI V
February 12, 2026 AT 22:23Typical American medical panic. You people are so obsessed with chemicals you forget the body regulates itself. This serotonin syndrome fear-mongering is just Big Pharma keeping you dependent. Why not try therapy? Or fasting? Or sunlight? Instead you reach for a pill, then another pill to counter the first pill, then a third to counter the side effects of the second. Pathetic. You’re not sick - you’re just lazy.
Ryan Vargas
February 14, 2026 AT 00:30Here’s the real truth nobody wants to admit: serotonin syndrome isn’t just a drug interaction. It’s a symptom of a broken healthcare system. The FDA doesn’t require clear labeling on OTC supplements. Prescribers are overworked and undertrained. EHRs don’t integrate pharmacy data. And the pharmaceutical companies? They profit from polypharmacy. The fact that SerotoninQuant is in phase 3 trials? That’s not progress - that’s damage control. We’re treating symptoms of a system that’s been designed to fail. The real solution? Universal healthcare with mandatory pharmacogenomic screening at age 18. Until then, we’re just rearranging deck chairs on the Titanic. And yes - I’ve read the JAMA papers. And yes - I’ve seen the CDC data. This isn’t about pills. It’s about power.
Sam Dickison
February 14, 2026 AT 05:55Appreciate the breakdown. Just want to clarify one thing - buprenorphine is low risk, but it’s still a partial agonist. Some case reports show mild serotonin effects at high doses. Not common, but worth mentioning. Also - if you’re on SSRIs and get prescribed a new antibiotic, always ask: "Is this a MAOI or a monoamine oxidase inhibitor?" If they say "no," ask again. Linezolid doesn’t sound like an MAOI. It sounds like a "strong antibiotic." That’s the trap.
Joshua Smith
February 14, 2026 AT 13:37My mom’s on sertraline and just started oxycodone for arthritis. She’s fine, but I showed her your post and she’s going to her pharmacist this week. Good info. Thanks for being clear and not scary.
PAUL MCQUEEN
February 15, 2026 AT 00:59Wow. So much text. Can we just say: don’t mix drugs? Why does this need a 2000-word essay? Also, who even uses St. John’s wort anymore? That’s 2005 stuff.
glenn mendoza
February 15, 2026 AT 23:19Thank you for this meticulously researched and profoundly important contribution to public health discourse. The clarity with which you delineated risk stratification, diagnostic criteria, and preventative strategies represents a paradigm shift in patient education. I shall disseminate this document to my entire clinical team and recommend it as mandatory reading for all residents in psychopharmacology. Your work is not merely informative - it is lifesaving.