When you hear radiation therapy, you might picture a scary machine or a long hospital stay. But what’s actually happening inside your body when those beams hit a tumor? It’s not magic. It’s biology. And it’s incredibly precise.
Radiation therapy doesn’t just burn cancer cells. It breaks them from the inside out-by targeting their DNA. Every cancer cell relies on its DNA to survive, divide, and spread. Radiation throws a wrench into that system. High-energy particles or waves-usually X-rays or protons-punch through skin and tissue until they reach the tumor. Once there, they don’t just knock things around. They smash the DNA inside cancer cells.
How Radiation Breaks DNA
The most damaging kind of DNA break is called a double-strand break. Imagine your DNA as a twisted ladder. Each strand is a side of that ladder. When radiation hits, it can snap both sides at the same spot. That’s a double-strand break. And that’s deadly for a cell.
Why? Because cells can’t fix this kind of damage easily. They have repair tools, sure. But when the break is too severe or too many happen at once, the cell gives up. It doesn’t just stop dividing-it dies. And that’s the goal: kill enough cancer cells so the tumor shrinks or disappears.
But radiation doesn’t just snap DNA directly. It also creates chaos in the cell’s environment. It splits water molecules inside the cell, turning them into reactive oxygen species-tiny, aggressive molecules that attack proteins, lipids, and DNA. This oxidative stress piles on top of the direct damage, making it even harder for the cell to survive.
What Happens After the Damage?
Cells don’t just die right away. They go through a series of internal alarms. When DNA breaks, special proteins like ATM and ATR spring into action. They sound the alarm: “DNA damaged!” The cell then pauses its life cycle-halting division to try and fix the damage.
It tries two main repair methods: non-homologous end joining (NHEJ) and homologous recombination (HR). NHEJ is fast but messy. It glues broken ends back together, often with errors. HR is more accurate-it uses a sister DNA strand as a template to rebuild the break. But here’s the twist: cancer cells that use HR often die quietly, without triggering any immune response.
That’s where new research changed everything. Scientists at the CMRI found that cancer cells with broken BRCA2 genes-common in some breast and ovarian cancers-can’t use HR properly. Instead, they die in a way that screams for help. They release signals that make the immune system think there’s an infection. That turns the tumor into a beacon for immune cells to attack.
This isn’t just theory. It’s changing how doctors combine radiation with immunotherapy. If you block HR in a tumor, you don’t just kill more cancer cells-you make the body help kill them too.
Why Some Cells Survive
Not all cancer cells die from radiation. Some are stubborn. One big reason? They’re starved for oxygen. Radiation needs oxygen to create the reactive molecules that cause the most damage. Tumors often have areas where blood flow is poor-hypoxic zones. In those spots, radiation can be up to three times less effective.
Another problem? Repair superpowers. Some cancer cells have extra copies of DNA repair proteins. Others turn on survival pathways that ignore the damage. A 2021 study showed that patients with head and neck cancer who had low levels of a repair protein called 53BP1 responded much better to radiation. Their tumors shrank more, and they lived longer. That means the body’s repair machinery can work against you.
And then there’s the tumor’s neighborhood. Surrounding cells-like fibroblasts and immune suppressors-can shield cancer cells, making them harder to kill. This microenvironment is now a major focus of research. You can’t just blast the tumor. You have to break its defenses too.
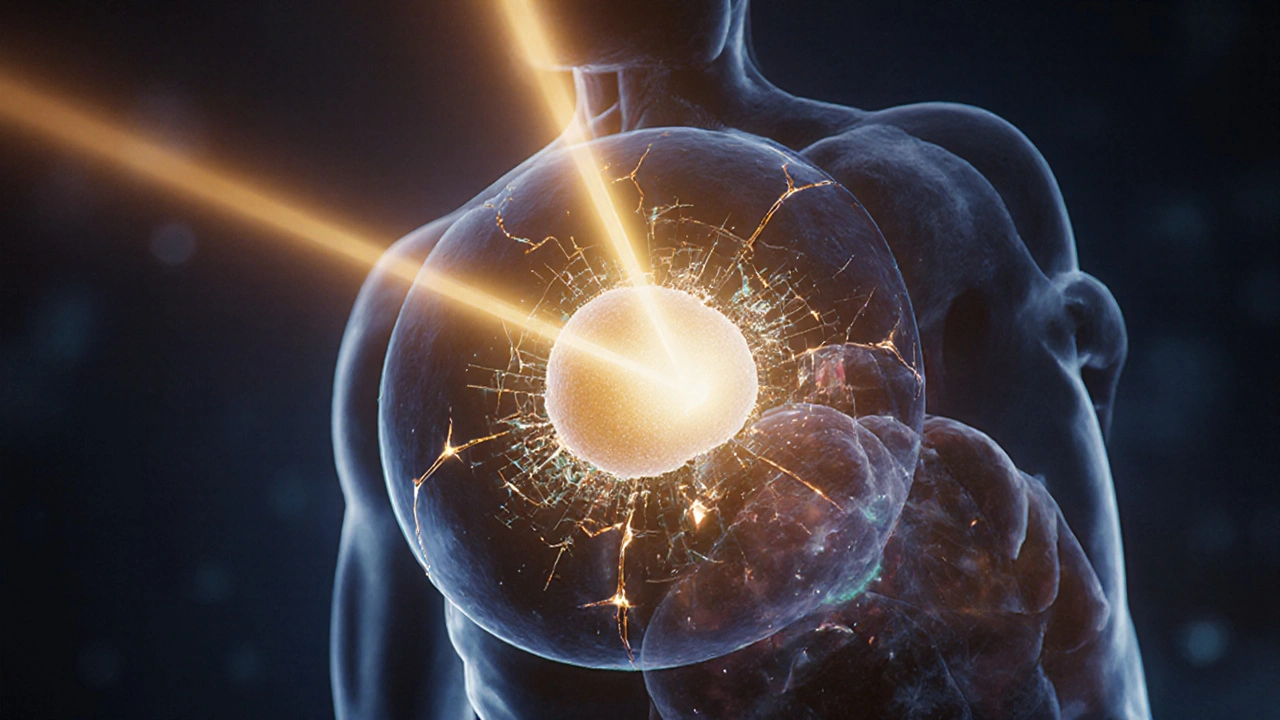
How Modern Radiation Avoids Hitting Healthy Tissue
It’s not just about hitting the tumor. It’s about missing everything else. That’s where techniques like IMRT and SBRT come in. IMRT shapes the radiation beam to match the tumor’s 3D outline, like a custom mold. SBRT delivers high doses in just a few sessions with pinpoint accuracy-down to less than a millimeter.
These methods rely on advanced imaging and AI. Before treatment, scans map the tumor’s exact location. During treatment, the machine tracks breathing and movement. If the tumor shifts, the beam adjusts in real time. This precision means fewer side effects. You’re not burning tissue-you’re surgically removing cells with beams.
The Immune System’s Role
For years, radiation was seen as a local treatment. It killed what it hit. But now we know it can have a body-wide effect. When cancer cells die in the right way-especially with high-dose, single-fraction treatments-they release signals that attract immune cells. They even change how they present their proteins on the surface, making them look more foreign to the immune system.
That’s why combining radiation with drugs like pembrolizumab (a checkpoint inhibitor) is working in trials. In one study, metastatic lung cancer patients who got both treatments saw their response rate jump from 22% to 36%. Radiation didn’t just kill cells. It turned the tumor into a vaccine.

The Ceramide Pathway and Blood Vessels
There’s another layer. Radiation doesn’t just target cancer cells. It hits the blood vessels feeding them. High-dose radiation triggers a molecule called ceramide to form in the lining of those vessels. Ceramide doesn’t just kill the endothelial cells-it cuts off the tumor’s supply line. Days after treatment, cancer cells in the center of the tumor starve and die from lack of oxygen and nutrients.
This is especially true in stereotactic ablative radiation (SABR), where doses are much higher than in traditional therapy. It’s not just a direct kill. It’s a slow suffocation.
What’s Next?
The future of radiation therapy isn’t just stronger beams. It’s smarter combinations. Researchers are testing drugs that block DNA repair-like PARP inhibitors-in patients with BRCA mutations. These drugs make cancer cells even more vulnerable to radiation.
Another breakthrough? FLASH radiotherapy. It delivers the entire dose in less than a second-faster than a blink. Early results show it kills tumors just as well but causes far less damage to healthy tissue. Human trials are underway.
And AI is speeding up planning. What used to take hours of manual work now takes under 10 minutes. Algorithms predict how a tumor will respond, letting doctors tailor doses before treatment even starts.
Radiation therapy isn’t just a tool. It’s a system-one that’s evolving from brute force to precision biology. We’re learning how to make cancer cells die in ways that wake up the immune system, cut off their food supply, and exploit their own weaknesses. The goal isn’t just to destroy. It’s to turn the body’s defenses into allies.
Why This Matters for Patients
If you’re considering radiation therapy, know this: it’s not one-size-fits-all. Your tumor’s genetics, oxygen levels, and repair capabilities all matter. That’s why doctors now test for markers like BRCA2 or 53BP1 before deciding on treatment. It helps them pick the best combo-radiation alone, radiation with immunotherapy, or radiation with a DNA repair blocker.
And while side effects still happen, modern techniques mean they’re milder. Fatigue, skin redness, or sore throat are common-but temporary. The days of massive scarring or organ damage are fading fast.
Radiation therapy isn’t the cure-all. But it’s one of the most effective tools we have. And now, with new science behind it, it’s becoming smarter, safer, and more powerful than ever.
Does radiation therapy hurt during treatment?
No, you don’t feel anything during the actual radiation delivery. It’s like getting an X-ray-you lie still, the machine moves around you, and you feel nothing. Any discomfort comes later, from side effects like skin irritation or fatigue, not the beam itself.
Can radiation therapy cure cancer?
Yes, in many cases. For early-stage cancers like prostate, cervical, or some lung cancers, radiation can be curative on its own. Even in advanced cases, it can shrink tumors, relieve pain, and extend life. It’s often used with surgery or chemo to improve outcomes.
Why do some tumors come back after radiation?
Some cancer cells survive because they’re resistant. They may have better DNA repair tools, live in low-oxygen areas, or have mutations that help them ignore damage. These surviving cells can regrow over time. That’s why researchers are now targeting resistance mechanisms with new drugs and combination therapies.
Is radiation therapy safe for older patients?
Yes. Radiation is often preferred for older adults because it’s less invasive than surgery and doesn’t require general anesthesia. Modern techniques minimize damage to healthy tissue, making it safer for people with other health conditions. Treatment plans are always adjusted for age, overall health, and tumor location.
How long does it take for radiation to kill cancer cells?
The damage happens instantly, but cells don’t die right away. Most cancer cells die over days or weeks as they try to divide with broken DNA. Some die during the first few treatments. Others hang on until they attempt to split, then fail and collapse. That’s why treatment is spread out over weeks-it catches cells at their most vulnerable moments.
Can radiation cause new cancers?
It’s possible, but rare. The risk is very low-less than 1 in 1000 over 10 years-and mostly seen in younger patients who receive high doses over large areas. For most people, the benefit of killing existing cancer far outweighs this small risk. Doctors use the lowest effective dose and avoid unnecessary exposure.
What’s the difference between radiation and chemotherapy?
Radiation targets a specific area, like a tumor in the lung or breast. Chemotherapy travels through your whole body. Radiation works by breaking DNA directly. Chemo uses chemicals to interfere with cell division. They’re often used together because they attack cancer in different ways.
Does radiation therapy make you radioactive?
No. External beam radiation-like IMRT or SBRT-does not make you radioactive. The radiation passes through you and is gone. You can safely be around others, including children and pregnant people, immediately after treatment. Only in rare cases, like with radioactive implants or injections, is temporary radioactivity a concern-and even then, it’s carefully managed.

Ross Ruprecht
November 22, 2025 AT 06:51So basically radiation is just fancy DNA vandalism? Feels like we're just throwing spaghetti at the wall and hoping some sticks.
Bryson Carroll
November 22, 2025 AT 23:34Stop pretending this is science it's just brute force with a fancy name. They don't know why it works they just know it kills stuff. And don't even get me started on the 'immune system activation' nonsense it's all correlation not causation
Lisa Lee
November 24, 2025 AT 23:03US medical tech is still the best in the world. No other country can do this kind of precision. Canada's healthcare system couldn't even handle this without a 6 month wait. Just sayin.
Jennifer Shannon
November 25, 2025 AT 10:57It's fascinating how radiation doesn't just kill-it transforms. The way it turns a tumor into an immunological beacon... it's almost poetic, isn't it? A biological symphony of destruction and awakening. The ceramide pathway, the BRCA2 vulnerability, the AI-guided precision-it's like the body's own defenses are being gently nudged into action, like waking a sleeping giant. And yet, we still treat it like a sledgehammer when it could be a scalpel woven with biology and intention. I wonder if we're underestimating the quiet dignity of cells choosing to die rather than persist in brokenness.
Suzan Wanjiru
November 26, 2025 AT 19:48Real talk-most patients don't care about HR or NHEJ. They care if it works and if they can still drive to work. The fact that modern RT lets people keep their jobs is huge. Also FLASH is gonna change everything, just wait.
Kezia Katherine Lewis
November 28, 2025 AT 18:02The mechanistic interplay between radiation-induced DNA damage, oxidative stress, and the tumor microenvironment is profoundly complex. The modulation of immune checkpoint dynamics via DAMPs released from immunogenic cell death represents a paradigm shift in radiotherapeutic oncology. We are no longer merely ablating tissue-we are reprogramming systemic antitumor immunity.
Henrik Stacke
November 29, 2025 AT 07:03Oh my goodness, this is absolutely brilliant. I mean, truly. The way you've laid this out-it’s like watching a masterclass in molecular warfare. I had no idea radiation could turn a tumor into a vaccine. I'm sitting here with tears in my eyes. This is the kind of science that makes you believe in humanity again.
Manjistha Roy
November 30, 2025 AT 07:00This is one of the clearest explanations I've ever read about radiation therapy. Thank you for taking the time to break down the science without oversimplifying. Many patients and families struggle to understand what's happening, and posts like this help bridge that gap. Keep sharing knowledge like this.
Jennifer Skolney
December 1, 2025 AT 20:07Wow this is so cool 😊 I had no idea radiation could make the body help fight cancer! That’s like giving your immune system a map to the bad guys. Also FLASH sounds like sci-fi but real?? Mind blown 💫
JD Mette
December 2, 2025 AT 17:39I appreciate how thorough this is. It’s easy to fear what you don’t understand, and this helps demystify a lot. I’ve seen people avoid treatment because they think it’s torture-this kind of clarity matters.
Olanrewaju Jeph
December 4, 2025 AT 00:30Excellent exposition of the biological mechanisms underlying radiation therapy. The integration of molecular biology with clinical outcomes is both elegant and clinically significant. One must acknowledge the strides made in image-guided adaptive radiotherapy and the emerging role of PARP inhibitors in radiosensitization. This is the future of precision oncology.