When you’re prescribed a biologic drug like Humira for rheumatoid arthritis or Crohn’s disease, you might assume that a cheaper version-called a biosimilar-is your best bet. After all, biosimilars are FDA-approved to work just like the original, and they can cost 10-33% less. But if you’ve tried to fill a prescription for one, you’ve probably run into a wall: prior authorization forms, stacked tiers, and insurers treating the cheaper option like it’s just as expensive as the brand-name drug.
Why Biosimilars Are Still Hard to Get, Even When They’re Approved
Biosimilars aren’t generics. They’re complex proteins made from living cells, not chemicals. That’s why they cost more to develop than a simple pill. But once they’re approved-like Zarxio in 2015, or the eight adalimumab biosimilars that hit the market by 2023-they’re supposed to drive down prices. And they do. But insurance companies often make it harder to use them than to stick with the original.In 2025, 99% of Medicare Part D plans put Humira and its biosimilars on the exact same tier. That means if Humira costs you $1,200 a month out-of-pocket, your biosimilar will cost $1,150. That $50 difference? Not enough to motivate most patients to switch, especially when the paperwork is the same.
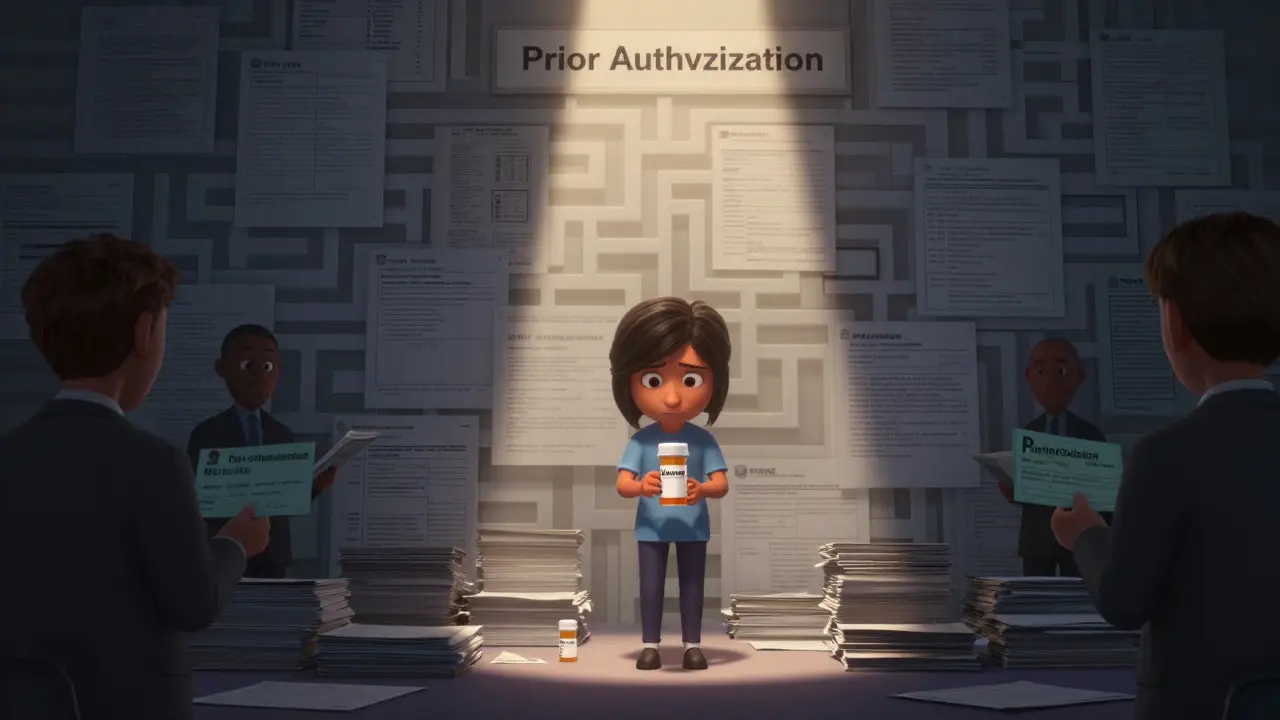
And that paperwork? Prior authorization is required for 98.5% of plans covering both Humira and its biosimilars. Not one plan made the biosimilar easier to get. In fact, many require you to try the biosimilar first-step therapy-before approving the original drug, even if your doctor says you’ve already failed it.
How Tier Placement Kills Incentive to Switch
Insurance plans use tiers to control costs. Tier 1: cheap generics. Tier 4 or 5: expensive biologics. Biosimilars almost always land in Tier 4 or 5, the same as the brand-name drug. That’s not a mistake. It’s a strategy.According to JAMA Network data from June 2024, only 1.5% of plans placed biosimilars on a lower tier than the reference product. That means patients pay the same coinsurance-often 25-33% of the drug’s list price-whether they take Humira or Cyltezo. If the drug costs $5,000 a month, you’re paying $1,250-$1,650 out of pocket. That’s a lot for anyone, but especially for seniors on fixed incomes.
Even worse: insulin biosimilars. Eight are approved. Only 10% of Medicare Part D plans cover them. Meanwhile, 80% cover the brand-name Lantus. Why? Because the manufacturer still pays rebates to pharmacy benefit managers (PBMs) to keep their product on formularies-even when cheaper alternatives exist.
What PBMs Are Really Doing (And Why)
Pharmacy Benefit Managers-Express Scripts, OptumRx, CVS Caremark-control which drugs get covered and at what cost. They’re not insurers. They’re middlemen paid by drugmakers to manage formularies. And they’ve got a conflict of interest.They get paid based on rebates from brand-name drugmakers. So even when biosimilars are cheaper, they’re not always profitable for PBMs. That’s why, as of 2025, three major PBMs excluded Humira from their standard commercial formularies-but only because they wanted to force patients onto their preferred biosimilars. That’s not helping patients. It’s just swapping one gatekeeper for another.
Express Scripts, for example, removed Humira entirely from its 2025 formularies and placed three biosimilars on Tier 3-slightly better than Tier 4. But patients still pay 25% coinsurance. No copay. No discount. Just a slightly less expensive version of the same pain.

Doctors Are Spending Hours on Paperwork, Not Patients
A 2024 survey by the Alliance for Patient Access found that 78% of rheumatologists spend 3-5 hours a week just filling out prior authorization requests. That’s time they could be seeing patients. And it’s not just one form. Each drug, each change, each denial requires a new submission.One case from the Rheumatology Advisor tells the story: a patient with severe rheumatoid arthritis was denied Humira because the plan required a 60-day trial of a biosimilar first. The patient waited 28 days. During that time, their joint damage worsened. The delay wasn’t clinical. It was administrative.
Specialty pharmacies are overwhelmed too. They handle 10-15 prior authorizations per patient per year for biologics. Many don’t have enough staff to keep up. Delays mean patients stop taking their meds. And that leads to hospitalizations, ER visits, and higher overall costs.
Why the U.S. Lags Behind Europe
In Europe, biosimilars make up over 80% of the market for drugs like Humira. In the U.S.? Just 23%. Why the gap?European countries use centralized pricing and mandatory substitution. If a biosimilar is approved, it’s automatically available at lower cost. No prior authorization. No tier games. No rebates to block access.
In the U.S., it’s the opposite. PBMs and drugmakers have built a system where the most expensive option stays on top-not because it’s better, but because it pays the most.
The Congressional Budget Office estimates biosimilars could save the U.S. $54 billion over the next decade. But under current coverage rules? Only $1.8 billion. That’s a $52 billion gap. And it’s not because patients don’t want cheaper options. It’s because the system is designed to keep them from getting them.

What’s Changing in 2025 (And What’s Not)
There are signs of movement. The Office of Inspector General (OIG) called out the lack of tier differentiation in 2024. CMS responded by expanding its monitoring of formulary practices. Some PBMs are now excluding originator drugs entirely to push biosimilars.But exclusion isn’t access. It’s coercion.
Real progress would mean:
- Biosimilars on lower tiers with lower coinsurance
- Eliminating prior authorization for biosimilars when the reference product is already approved
- Banning step therapy that forces patients to try a cheaper drug first, even if it’s clinically inappropriate
- Requiring PBMs to report how many biosimilars they cover-and at what tier
The Inflation Reduction Act gave CMS the power to enforce this. But so far, enforcement is light. No penalties. No audits. No public consequences for plans that treat biosimilars like second-class drugs.
What Patients Can Do Right Now
If you’re stuck with a high-cost biologic and your doctor recommends a biosimilar:- Ask your doctor to write a letter of medical necessity explaining why the biosimilar is appropriate
- Call your insurer and ask: "Is the biosimilar on a lower tier? If not, why?"
- Request a formulary exception or appeal if your request is denied
- Check if your state has laws requiring biosimilar substitution at the pharmacy level
Some states, like California and New York, have passed laws allowing pharmacists to substitute biosimilars without prescriber approval-similar to generics. But even there, insurers can still block it with prior authorization.
Bottom line: the system isn’t broken. It’s working exactly as designed-to protect profits, not patients.
What’s Next?
Biosimilars are here to stay. By 2027, market share could hit 40% if PBMs keep excluding originators. But unless tier placement changes, patients won’t see real savings. And without real savings, the promise of biosimilars-lower costs, better access, fair competition-will remain just a promise.Until then, if you’re paying $1,200 a month for a drug that could cost $800, you’re not getting a bargain. You’re getting a system that still treats cheaper as the same as expensive.
Are biosimilars as safe as brand-name biologics?
Yes. Biosimilars are approved by the FDA after rigorous testing to prove they’re highly similar to the original biologic in safety, purity, and effectiveness. They undergo the same clinical trials and monitoring. The FDA has approved over 70 biosimilars since 2015, and real-world data shows no increase in adverse events compared to the reference products.
Why don’t insurers put biosimilars on lower tiers?
Because pharmacy benefit managers (PBMs) receive rebates from brand-name drugmakers to keep their products on preferred tiers. Lowering the tier for biosimilars would reduce those rebates. Even though biosimilars cost less, they don’t pay enough back to PBMs to make it worth their while. That’s why 99% of Medicare plans put them on the same tier as the original.
Can my pharmacist switch me to a biosimilar without my doctor’s approval?
Only if the biosimilar is designated as "interchangeable" by the FDA and your state allows substitution. As of 2025, only a few biosimilars have interchangeable status, and even then, insurers can block substitution with prior authorization. Most states don’t have clear rules, so pharmacists often can’t make the switch without a new prescription.
Why is prior authorization required for biosimilars if they’re approved?
Prior authorization isn’t about safety-it’s about cost control. Insurers use it to delay or deny access, even for FDA-approved drugs. For biosimilars, it’s often used to force patients to try the brand-name drug first, or to ensure the prescriber has documented "failure" of other treatments. It’s a barrier, not a safeguard.
Do biosimilars save money for patients?
Only if the insurer lets them. If a biosimilar is on the same tier as the brand-name drug, patients pay almost the same out-of-pocket cost-often $1,150-$1,200 a month. The real savings go to insurers and PBMs, not patients. True savings happen only when biosimilars are on lower tiers with fixed copays, not percentage coinsurance.

Chris Urdilas
January 28, 2026 AT 05:27So let me get this straight - we’ve got cheaper, FDA-approved drugs that work just as well, but insurers make you jump through 17 hoops just to get them? And the only people saving money are the middlemen? Brilliant. Absolute genius. Someone get this man a Nobel Prize in Corporate Logic.
matthew martin
January 28, 2026 AT 23:06I’ve been on Humira for six years. My doc pushed me to switch to a biosimilar last year - said it was identical. So I did. Got stuck in prior auth hell for 47 days. My joints screamed. My bank account cried. Meanwhile, my insurer’s CEO bought a yacht. Coincidence? Nah. This isn’t broken - it’s engineered. And honestly? I’m tired of being the collateral damage in someone’s quarterly earnings report.
My pharmacist told me they’re not even allowed to substitute unless it’s labeled ‘interchangeable’ - and even then, the plan blocks it. So we’re stuck in this weird limbo where the science says ‘yes’ but the system says ‘no thanks, we’re good.’
It’s not just about money. It’s about dignity. You’re not asking for luxury. You’re asking to not be punished for wanting to live without constant pain. And yet, we treat patients like frauds before we treat them like humans.
Europe does it right. They don’t play games. They just say, ‘Here’s the cheaper version - take it.’ And guess what? People get better. Costs drop. Everyone wins except the people who profit from the chaos.
I don’t care if you’re a PBM exec or a senator. If you’re okay with this, you’re not protecting the system - you’re protecting your paycheck while people bleed out in waiting rooms.
Katie Mccreary
January 29, 2026 AT 10:54OMG I literally just got denied for my biosimilar because ‘they need to confirm you’ve tried Humira first’ - but I’ve been on it for 4 years and it’s destroying my liver. So now I have to wait 3 weeks to get the drug that’s literally the same but cheaper? This is dystopian fanfic.
Mel MJPS
January 30, 2026 AT 02:31My mom’s on insulin. She pays $1,100 a month for Lantus. There’s a biosimilar that costs $300. Her plan won’t cover it unless she fills out a 12-page form and gets a letter from her endocrinologist… which takes 3 weeks. She’s 72. She can’t do this. I had to quit my job to help her navigate this mess. This isn’t healthcare. It’s a maze built by wolves.
Rhiannon Bosse
January 30, 2026 AT 09:52So the real villain here isn’t the drug companies… it’s the PBMs? Wait, let me guess - they’re secretly owned by Big Pharma who also owns the insurers who own the pharmacies who own the lobbyists who own Congress? 😏 And we’re all just pawns in a game where the only rule is ‘make patients suffer but keep the money flowing.’ I’m not even mad. I’m just impressed. Like, ‘wow, you really built a machine to extract pain and profit simultaneously.’ Bravo. 🎭
Jeffrey Carroll
January 31, 2026 AT 08:05The structural barriers to biosimilar adoption are not merely administrative; they represent a systemic misalignment of incentives within the pharmaceutical supply chain. The current reimbursement model, heavily reliant on rebate structures, disincentivizes cost-reducing innovation. This is not an oversight - it is a feature of a market-driven system that prioritizes financial intermediation over patient welfare. Meaningful reform requires legislative intervention to decouple formulary placement from rebate economics.
Rose Palmer
February 2, 2026 AT 05:32As a healthcare advocate, I want to emphasize that while the system is flawed, there are actionable steps patients can take. Requesting a formulary exception, documenting medical necessity with your provider, and contacting your state’s insurance commissioner can create real change. Many patients don’t realize they have more power than they think - and collective advocacy has already forced PBMs to adjust formularies in several states. Don’t give up. Your voice matters.
Phil Davis
February 2, 2026 AT 18:58They say biosimilars are ‘just as good.’ But if they’re so good, why do I need a PhD to get one? Why does my doctor have to write a novel just to prescribe something that’s literally the same? It’s not about safety. It’s about control. And control means profit. The FDA says it’s safe. The science says it’s equal. The system says ‘nope, not today.’
Bryan Fracchia
February 4, 2026 AT 10:14You know what’s wild? We don’t have this problem with insulin in Canada. Or with Humira in Germany. We’re not ‘special’ here. We’re just the only country that treats healthcare like a stock market. And if you’re not profitable, you’re not worth treating. It’s not capitalism - it’s capitalism with a scalpel to the throat of the sick.
I used to think the system was broken. Now I think it’s working perfectly… for the people who designed it.
Irebami Soyinka
February 4, 2026 AT 11:58USA still thinks it's the best? 😂 Look at this mess - you let corporations run your medicine like a casino! In Nigeria, we don't have this nonsense - if a drug is approved, you get it. No 12-page forms, no 'step therapy' nonsense. You people built the internet but can't fix a drug system? 🤦♀️ You're not advanced - you're just rich and lazy. Fix your system or stop pretending you're the world's leader in anything!
And don't even get me started on PBMs - they're like vampires with spreadsheets. 😤
SRI GUNTORO
February 4, 2026 AT 12:39It’s obvious. People who can’t afford these drugs shouldn’t be taking them in the first place. If you can’t pay, you shouldn’t be sick. This is why we need to stop enabling laziness and poor lifestyle choices. Maybe if you ate better and exercised, you wouldn’t need these expensive drugs. The system isn’t the problem - you are.