Every year, hundreds of thousands of patients in U.S. hospitals suffer harm because of medication errors-many of them preventable. It’s not just about a nurse giving the wrong dose. It’s about systems failing at every step: from the doctor writing the order, to the pharmacy filling it, to the nurse handing it to the patient. The truth is, medication safety isn’t about being perfect. It’s about building layers of protection so that even when someone makes a mistake, the system catches it before the patient pays the price.
What Counts as a Medication Error?
A medication error isn’t just giving the wrong pill. It’s giving the right drug at the wrong time, in the wrong dose, to the wrong person-or giving it the wrong way. The American Society of Health-System Pharmacists defines it as any preventable event that leads to inappropriate use or patient harm. That includes mislabeled vials, unclear handwriting on paper orders, confusing drug names like hydralazine and hydroxyzine, or even giving a drug meant for weekly use every day.
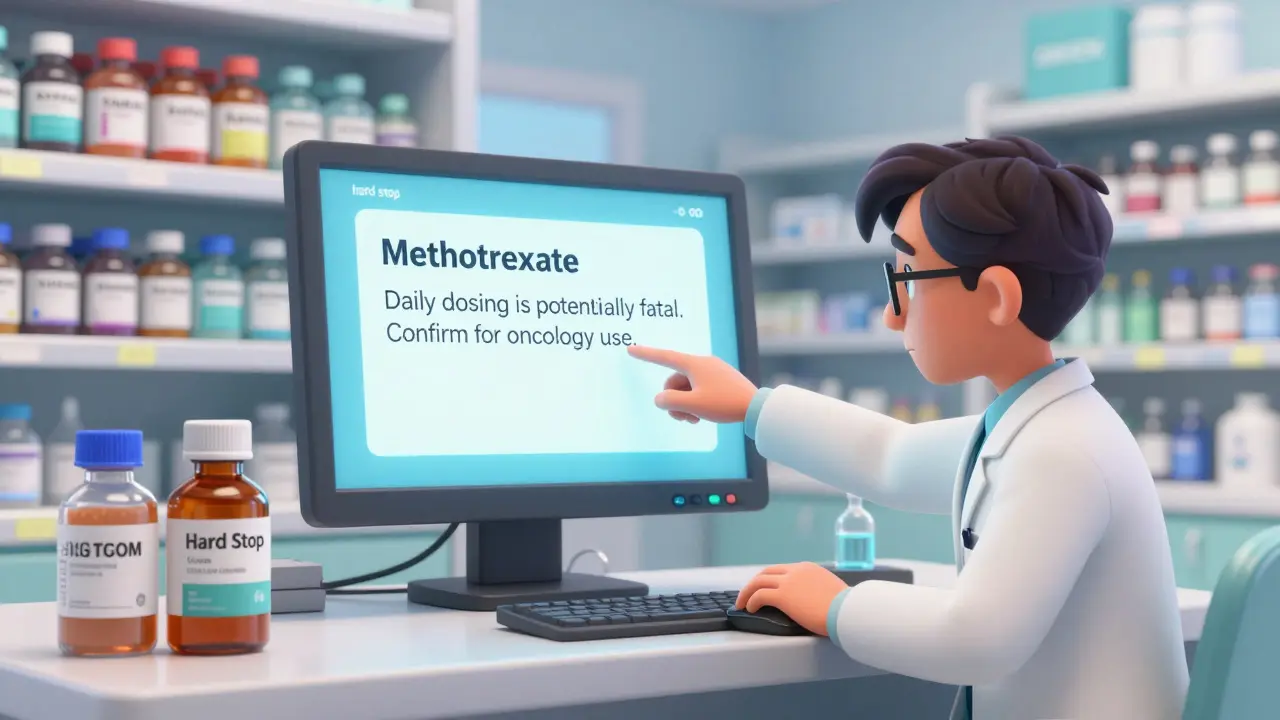
One of the most infamous examples is methotrexate. This drug is used for cancer and autoimmune diseases. When given weekly, it’s life-saving. When given daily by accident, it’s deadly. In 2006, a 17-year-old girl died after being prescribed daily methotrexate instead of weekly. Her chart had no warning. The pharmacy didn’t catch it. The nurse didn’t question it. That’s not negligence-it’s a system failure.
The Big Players in Medication Safety
Three major organizations shape how hospitals protect patients: the Institute for Safe Medication Practices (ISMP), The Joint Commission, and the American Society of Health-System Pharmacists (ASHP).
ISMP’s Targeted Medication Safety Best Practices for Hospitals (2020-2021) is the most detailed roadmap. It lists 19 specific actions hospitals must take. For example: block daily dosing of methotrexate unless the prescriber confirms it’s for cancer. Remove glacial acetic acid from hospital floors-it looks like water but can burn skin. Prevent vinca alkaloids from being given into the spinal fluid-this causes paralysis or death.
The Joint Commission sets national patient safety goals. They require hospitals to reconcile medications when patients move between units or get discharged. That means checking every single drug the patient was on before, during, and after their stay. It sounds simple, but in busy ERs and ICUs, it often gets skipped.
ASHP focuses on high-alert medications-drugs that can cause serious harm if misused. These include insulin, opioids, anticoagulants, and IV potassium. ASHP says these drugs need three things: standardized concentrations, automated dose checks, and independent double-checks before administration.
Technology That Actually Saves Lives
Barcode scanning isn’t just for grocery stores. In hospitals, every medication dose should be scanned at the bedside. The system checks: Is this the right patient? Is this the right drug? Is this the right dose? Is this the right time? If any part is wrong, the scanner beeps and stops the process.
That’s not optional anymore. By 2022, 89% of large U.S. hospitals had barcode systems. But only 54% of small hospitals did. Why? Cost. Training. Outdated electronic health records.
Hard stops in computer systems are even more powerful. When a doctor tries to order daily methotrexate, the system pops up: “This is a weekly dose. Confirm this is for cancer treatment.” Only if they click “Yes” and type a reason does the order go through. Since these hard stops were introduced, an estimated 1,200 serious errors have been prevented each year, according to Dr. Robert Wachter at UCSF.
But tech alone isn’t enough. A nurse in a rural hospital told the American Nurses Association that requiring both written and verbal discharge instructions for methotrexate created delays during staffing shortages. The system was designed to protect patients-but it didn’t account for real-world pressure.
Human Factors Still Matter Most
Even with perfect technology, people make mistakes. Fatigue. Distractions. Pressure to move patients quickly. That’s why culture matters more than any checklist.
One hospital in Ohio implemented a “stop if unsure” policy. Nurses were told: If anything feels off-even if you can’t explain why-stop. Call the pharmacist. Ask the doctor. No one gets in trouble for pausing. Within three months, near-miss errors dropped by 40%.
Patients also play a role. A 2022 survey by the National Council on Aging found that 68% of adults over 65 felt safer when staff checked their name, birth date, and wristband before giving any drug. Simple. Low-tech. Effective.
But there’s a dark side. One ICU nurse posted on Reddit about a neuromuscular blocker error that led to patient harm. The hospital had all the right systems: double-checks, barcodes, alerts. But the team was so used to overriding them that they didn’t question the system anymore. That’s called “automation bias”-trusting the machine too much, even when it’s wrong.
What Happens When Systems Fall Short?
Not every hospital has the budget for advanced tech. Community hospitals with fewer than 100 beds are 36% less likely to have full ISMP best practices in place than academic medical centers. Many still use paper orders. Some still store high-risk drugs like insulin and morphine in the same drawer.
When systems fail, the cost isn’t just human-it’s financial. Medication errors cost U.S. hospitals an estimated $21 billion a year. That’s more than the annual budget of many small states. CMS now ties hospital payments to safety performance. If you have too many errors, you get paid less.
And it’s getting worse outside the hospital. Between 2018 and 2022, medication errors in outpatient clinics rose by 47%. Patients are getting prescriptions filled at pharmacies, managing multiple drugs at home, and often don’t understand what they’re taking. That’s why ISMP is expanding its best practices to include ambulatory care in 2024.

What’s Next for Medication Safety?
Artificial intelligence is starting to help. By 2025, 75% of U.S. hospitals are expected to use AI to flag risky prescriptions in real time-like spotting when a patient is getting two drugs that cause dangerous interactions.
The FDA is requiring clearer labeling on high-concentration electrolytes by the end of 2024. The AHRQ wants to cut opioid-related harm by 50% by 2027. And pilot programs at Mayo Clinic and Johns Hopkins are asking patients: “Do you know why you’re taking this drug?” When patients answer correctly, error detection improves by 32%.
But the biggest change won’t come from tech or regulations. It’ll come from culture. When staff feel safe speaking up-when pharmacists aren’t afraid to question a doctor, when nurses aren’t rushed into giving a drug, when patients are treated as partners, not passive recipients-then safety becomes real.
Medication safety isn’t about having the fanciest system. It’s about having a team that cares enough to slow down, ask questions, and never assume.
What are high-alert medications, and why are they dangerous?
High-alert medications are drugs that carry a higher risk of causing serious harm if used incorrectly. Examples include insulin, opioids like morphine, anticoagulants like heparin, and IV potassium. A small mistake-like giving 10 units instead of 1, or confusing two similar-looking vials-can lead to coma, organ failure, or death. Hospitals must use extra safeguards: standardized concentrations, automated dose checks, and independent double-checks before administration.
How does the ISMP methotrexate hard stop work?
The ISMP hard stop for methotrexate blocks any order for daily dosing unless the prescriber confirms it’s for cancer treatment. When a doctor types in methotrexate, the system defaults to weekly dosing. If they try to change it to daily, a pop-up appears: “Daily methotrexate is potentially fatal. Confirm this is for oncology use.” The doctor must select a reason from a dropdown and type a note. Only then can the order proceed. Since this was implemented, an estimated 1,200 serious errors have been prevented each year.
Why do barcode scanning systems reduce errors?
Barcode scanning creates a final safety check at the bedside. Before giving a drug, the nurse scans the patient’s wristband and the medication’s barcode. The system compares: Is this the right patient? Is this the right drug? Is this the right dose? Is this the right time? If anything doesn’t match, the scanner beeps and won’t allow administration. This stops errors caused by look-alike drugs, wrong patient IDs, or misread orders. Hospitals using full barcode systems see 55% fewer serious medication errors.
What’s the biggest challenge in implementing medication safety systems?
The biggest challenge isn’t technology-it’s culture and workflow. Many hospitals have the tools but lack consistent use. Staff get used to overriding alerts, or feel pressured to move quickly. Small hospitals struggle with budget and outdated EHR systems. A 2021 survey found 63% of hospitals had trouble creating hard stops because their EHR vendor didn’t support it. Training takes time, and staff turnover makes it harder to keep everyone on the same page.
Can patients help prevent medication errors?
Absolutely. Patients who ask questions and double-check their medications are less likely to be harmed. Studies show that 68% of older adults feel safer when staff verify their name, birth date, and wristband before giving any drug. Patients should always know: Why am I taking this? What does it do? What are the side effects? They should bring a list of all their medications to every appointment and ask the pharmacist to review it. Simple actions like these reduce errors significantly.
Are medication errors more common in clinics than hospitals?
In recent years, yes. While hospitals have better systems, outpatient clinics have seen a 47% rise in reported medication errors between 2018 and 2022. Why? Patients manage multiple prescriptions at home. Prescriptions are sent electronically but not always reviewed. Pharmacists are overloaded. Doctors have limited time to explain. ISMP is now expanding its safety guidelines to include ambulatory care settings to address this growing problem.
What You Can Do Today
If you’re a patient: Always ask, “What is this for?” and “How do I take it?” Keep a list of every drug you take-including vitamins and supplements-and bring it to every appointment. If something looks different from last time, say so.
If you’re a healthcare worker: Don’t rush. If you’re unsure, stop. Ask. Double-check. Use your system. Don’t override alerts just because it’s faster. Your hesitation might save a life.
If you’re a hospital leader: Invest in training, not just tech. Make it safe for staff to speak up. Celebrate near-miss reports-not as failures, but as opportunities to fix the system.
Medication safety isn’t a project with an end date. It’s a habit. And like any habit, it only works when everyone-patients, nurses, doctors, pharmacists-keeps showing up for it.


Dana Termini
January 6, 2026 AT 00:39Every time I see a story like this, I think about my mom’s hospital stay last year. They gave her the wrong blood thinner because the barcode didn’t scan, and the nurse just clicked through the alert. She ended up in the ICU for three days. No one got fired. No one even apologized. Just another ‘oops’ in the system.
Wesley Pereira
January 6, 2026 AT 22:51Let’s be real-hard stops are great until you’re the one who needs to give a life-saving dose at 3 AM and the system’s down. We’ve got EHRs that were coded in 2011 and vendors who treat ‘urgent fixes’ like a suggestion. And don’t even get me started on the ‘double-check’ that’s just two tired nurses nodding at each other while scrolling TikTok. Automation bias? Nah, it’s just burnout with a fancy name.
Stuart Shield
January 8, 2026 AT 12:12It’s like watching a house built with bricks and glue-some parts are solid, others are held together by duct tape and hope. The tech’s brilliant, sure-barcodes, AI flags, hard stops-but if the culture says ‘just bypass it,’ then you’ve got a cathedral with a leaky roof and everyone pretending it’s raining indoors on purpose. We need to stop treating safety as a checklist and start treating it like a sacred promise.
Lily Lilyy
January 9, 2026 AT 06:57Everyone can help. Patients, nurses, doctors, pharmacists. Just ask questions. Just pause. Just care. Small things make huge differences. Be kind. Be brave. Be present. Safety starts with you.
Tom Swinton
January 10, 2026 AT 11:11Okay, so let’s unpack this-because honestly, the real issue isn’t just the tech or even the training, it’s the entire institutional inertia that prioritizes throughput over safety, and let me tell you, when you’re running 12-hour shifts with three patients and a broken printer and a manager who thinks ‘efficiency’ means cutting staff by 20%, no amount of barcode scanners is going to fix the fact that people are emotionally and physically exhausted, and when you’re exhausted, you don’t think, you react, and reactions are where mistakes happen, and mistakes in med administration aren’t just errors-they’re tragedies waiting to happen, and yes, I’ve seen it, I’ve been there, and I’ve had to call a code because someone gave IV potassium too fast because the alert was ‘just another pop-up’-and that’s not negligence, that’s systemic collapse, and we’re all just trying to survive it.
Gabrielle Panchev
January 12, 2026 AT 08:40Wait-so we’re blaming the nurses for overriding alerts? But who designed the system that floods them with 17 alerts per dose, 8 of which are for drugs they’ve given 100 times without incident? Who decided that a ‘hard stop’ for methotrexate should require a 3-step confirmation process that takes 45 seconds when the patient is crashing? And who’s the genius who thinks patients should ‘ask why they’re taking it’ when 60% of them are on 8+ meds and can’t tell the difference between lisinopril and losartan? This isn’t safety-it’s performative bureaucracy with a side of victim-blaming.
Melanie Clark
January 12, 2026 AT 19:30Big Pharma is behind all of this. They want you dependent on meds. They pay the EHR companies to make alerts annoying so you override them. They profit from errors because more people end up in the hospital again. The ‘weekly methotrexate’ thing? That’s a cover-up. The real danger is the lithium in the water supply. And why do you think they removed glacial acetic acid? Because it’s a natural antiseptic and they don’t want you healing without a prescription. Trust nothing. Question everything. They’re watching.
Saylor Frye
January 14, 2026 AT 09:20Look, I get the vibe. But let’s be honest-this is just another ‘healthcare is broken’ op-ed dressed up like a whitepaper. Everyone knows the system’s flawed. The real question is: why do we keep pretending that adding another checklist or scanning a barcode is going to fix a culture that’s been corroded by profit motives and bureaucratic inertia for decades? Spoiler: it won’t. We’re just rearranging deck chairs on the Titanic while the CFO gets a bonus.
Isaac Jules
January 15, 2026 AT 12:53Wow. So we’ve got a 17-year-old girl dead because someone didn’t read the chart? And you’re surprised? 😒 This isn’t a ‘system failure’-it’s negligence on a national scale. Nurses don’t question orders? Doctors don’t double-check? Pharmacies are understaffed? That’s not a flaw-it’s incompetence. And now you want to blame ‘automation bias’? Nah. Blame the people who didn’t care enough to learn their job. And if your hospital still uses paper orders? You’re not a healthcare provider-you’re a liability waiting to happen. 🔥