Every year, the world spends more on healthcare - and a big chunk of that goes to prescription drugs. In 2025, global health spending is expected to hit $1.6 trillion in medicine sales alone, not counting the $157 billion poured into COVID-19 vaccines. But here’s the twist: while new, brand-name drugs keep pushing prices up, generics are the quiet force keeping the system from collapsing under its own weight.
Why Generics Matter More Than You Think
Generics aren’t just cheaper copies. They’re the reason millions of people can still afford insulin, blood pressure pills, or antibiotics. In high-income countries like the U.S., Canada, and Germany, generics make up 80 to 90% of all prescriptions filled. But they only account for about 20% of total drug spending. That’s because they cost a fraction of the original brand drugs - sometimes less than 10%.
Take the U.S., where drug spending jumped from $437 billion to $487 billion in 2024. That $50 billion increase came mostly from new, expensive treatments for cancer, obesity, and autoimmune diseases. But without generics, that number could’ve been $700 billion. Generic versions of drugs like Lipitor, Nexium, and Advil saved patients and insurers hundreds of billions over the last decade.
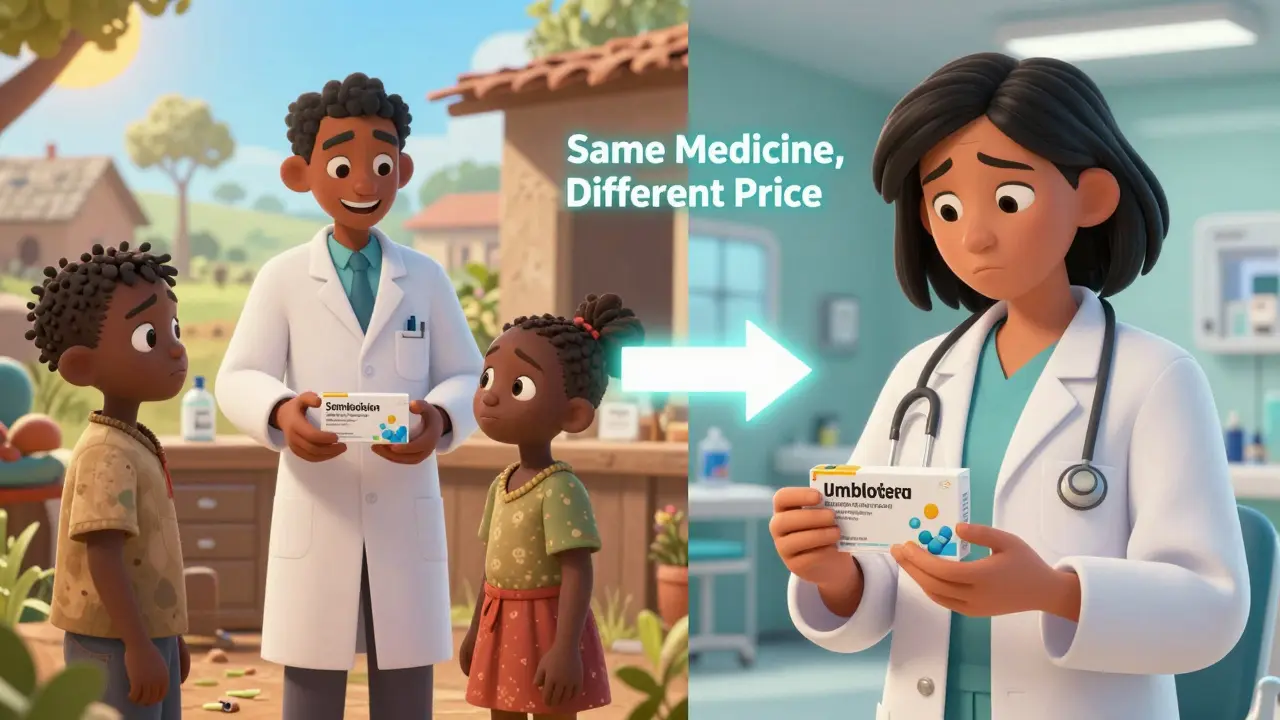
The Global Divide in Access
But not every country benefits equally. In 2022, 55 countries relied on people paying out of pocket for most of their healthcare. In Turkmenistan, Afghanistan, and Nigeria, those out-of-pocket costs made up more than 75% of total spending. When a person has to pay $50 for a month’s supply of a brand-name diabetes drug, they skip doses - or skip treatment entirely.
That’s where generics change lives. In low-income countries, generics are often the only viable option. The WHO reports that in places like Malawi and Lebanon, public healthcare spending dropped by 40% or more after the pandemic. Without cheap generics, those health systems would’ve collapsed. In fact, in many African and South Asian nations, over 90% of medicines used are generics - not because they’re preferred, but because there’s no other choice.
Where Generics Are Losing Ground
Generics aren’t winning everywhere. In emerging markets like China, India, and Brazil, there’s a shift happening. As incomes rise and health systems expand, more people are asking for the latest brand-name drugs - even if they’re expensive. China’s pharmaceutical market is growing fast, not because of generics, but because of increased access to innovative treatments. This trend is called the "pharmerging" effect: countries moving from basic access to advanced care.
But even in these countries, generics still play a role - just a different one. Instead of being the main source of treatment, they’re now used as backup options after brand drugs fail, or when patients can’t afford the newer versions. It’s a transition from survival to choice.
The Biosimilar Challenge
Some drugs can’t be copied easily. Biologics - drugs made from living cells, like Humira or Enbrel - are complex. Their copies are called biosimilars, and they’re harder to make, test, and approve. That’s why they’re slower to enter the market and often cost 15-30% less instead of 80-90% like traditional generics.
In the U.S., only a handful of biosimilars have launched for major biologic drugs. Insurers and doctors are still cautious. In Europe, adoption is higher, but even there, many patients get stuck on brand-name biologics because of prescribing habits and lack of education. This gap is growing as new biologics for Alzheimer’s, rare cancers, and autoimmune diseases hit the market - and prices keep climbing.
Who’s Paying the Bill?
Healthcare spending isn’t just about drugs. Hospitals, doctors, and tech account for most of the cost. But drug spending is the fastest-growing part. In the U.S., CMS projects drug costs will jump from $776 billion in 2025 to $1.7 trillion by 2033. Out-of-pocket costs for patients? They’re expected to rise from $177 per person in 2025 to $231 by 2033 - a 30.5% increase.
And it’s not just the U.S. Insurers in the Middle East and Africa report medical cost growth of 12.1% in 2025 - the highest in the world. In Asia Pacific, it’s 12.3%. These increases are driven by new technologies, aging populations, and rising demand for mental health services - where generic antidepressants and antipsychotics could help, but aren’t always used.
Meanwhile, global aid for health is falling. In 2025, development assistance for health is projected to drop to $39.1 billion - the lowest since 2009. That means low-income countries can’t rely on foreign help anymore. Their only tool to keep care affordable? Generics.
Why Generics Are Still the Best Bargain
Even with all the new drugs and rising costs, generics remain the most effective way to control spending. The WTW Global Medical Trends Survey found that 69% of insurers blame new medical technologies for rising costs - not generics. In fact, generics are the only thing holding back even steeper increases.
Consider this: if the U.S. didn’t have generics, its total drug spending in 2025 could’ve been $1.2 trillion instead of $776 billion. That’s $424 billion saved in one country alone. In the EU, generic use cuts drug spending by 40-50% compared to what it would be with only brand-name drugs.
And it’s not just about money. Generics keep people on treatment. A study in the U.K. showed that when patients switched from a brand-name statin to its generic version, adherence improved by 12%. Why? Because they could actually afford it.

The Future of Generics
Generics aren’t going away. But their role is changing. In rich countries, they’re now part of a smarter system - used to stretch budgets, support value-based care, and reduce patient burden. In poorer countries, they’re still the lifeline.
But there’s a risk. If governments don’t enforce strong generic substitution policies, if regulators delay approvals, or if pharmacies and doctors stick with brand names for kickbacks or habit, then the savings vanish. Countries like Thailand and Brazil have shown that with the right policies - mandatory generic prescribing, public education, and transparent pricing - generics can cover 95% of prescriptions without sacrificing quality.
The real question isn’t whether generics work. It’s whether the world will let them work.
What’s Holding Generics Back?
There are three big barriers:
- Patent evergreening: Drug companies make small changes to old drugs - like a new coating or dosage - to extend patents and block generics for years longer than intended.
- Slow regulatory approval: In some countries, it takes over two years to approve a generic drug, even if it’s already approved elsewhere. That delays savings.
- Prescriber resistance: Many doctors still write brand-name prescriptions out of habit, fear of liability, or influence from pharmaceutical reps.
Fixing these isn’t complicated. Countries that require pharmacists to substitute generics unless the doctor writes "do not substitute" see much higher use. Places like Sweden and Germany have done this for over a decade - and saved billions.
What You Can Do
If you’re in a country where generics are available:
- Ask your doctor if a generic version exists for your prescription.
- Check your pharmacy’s formulary - many have tiers, and generics are usually the cheapest.
- If you’re on Medicare or private insurance, ask about preferred generic drugs - they often have lower copays.
If you’re a policymaker, advocate, or health worker: push for mandatory substitution laws, faster generic approvals, and public campaigns that build trust in generic quality. The WHO has shown that when people know generics are safe, they use them.
Are generic drugs as safe as brand-name drugs?
Yes. Generic drugs must meet the same strict quality, strength, purity, and performance standards as brand-name drugs. In the U.S., the FDA requires generics to have the same active ingredients and work the same way in the body. Studies show they’re equally effective in treating conditions like high blood pressure, diabetes, and depression. The only differences are in inactive ingredients - like fillers or dyes - which don’t affect how the drug works.
Why are some generic drugs more expensive in certain countries?
It’s not about the drug itself - it’s about the system. In countries with weak regulation, few manufacturers, or poor distribution networks, generics can cost more due to lack of competition. In places like Nigeria or Afghanistan, importing generics can be expensive because of tariffs, taxes, and broken supply chains. Even when a pill costs 10 cents to make, the final price to the patient might be $5 because of middlemen and logistics.
Do generics cause more side effects?
No. Generic drugs are required to have the same bioavailability as brand-name versions - meaning they’re absorbed into the bloodstream at the same rate and to the same extent. Side effects come from the active ingredient, not the filler. If a patient has a reaction, it’s almost always because of the drug itself, not because it’s generic. In fact, many patients report fewer side effects when switching to generics because they’re taking the drug consistently - something they couldn’t afford before.
Why don’t all doctors prescribe generics?
Some don’t know the options. Others are influenced by pharmaceutical marketing. A few worry about liability if a patient has a problem - even though there’s no evidence generics are riskier. In countries without automatic substitution laws, doctors often write brand names out of habit. Patient education helps. When patients ask for generics, doctors are more likely to prescribe them.
Can generics be used for chronic conditions like diabetes or heart disease?
Absolutely. In fact, generics are the backbone of chronic disease management. Metformin for diabetes, lisinopril for high blood pressure, and atorvastatin for cholesterol are all generics used by millions worldwide. Studies show patients on generic chronic meds are more likely to stick with treatment because they can afford it - which leads to fewer hospital visits and better outcomes.
Is the quality of generics from India or China reliable?
Yes, if they’re approved by strict regulators. Many top generic manufacturers in India and China supply drugs to the U.S., EU, and WHO. The FDA and EMA inspect these facilities regularly - and many meet or exceed Western standards. The problem isn’t the country of origin - it’s unregulated suppliers. Always choose generics from reputable distributors and avoid online pharmacies that don’t require prescriptions.


Jasmine Yule
December 29, 2025 AT 18:36Generics saved my life. I’m on metformin and lisinopril - both generics. My copay is $3. If I had to pay brand prices, I’d be choosing between meds and groceries. This isn’t just economics - it’s survival.
Jim Rice
December 30, 2025 AT 18:30Stop romanticizing generics. They’re not magic. I’ve seen patients have weird reactions - not because of the drug, but because the fillers are different. And let’s be real: most doctors don’t even know what’s in the generic versions they prescribe. It’s a gamble.
Manan Pandya
December 31, 2025 AT 16:00As someone from India, I’ve seen the raw power of generics. Our pharma industry produces over 60% of the world’s vaccines and 20% of its generic drugs. The quality? Often better than Western brands - regulated by WHO, FDA, and EMA. The real issue isn’t the pills - it’s the broken supply chains and corruption that inflate prices locally. Fix logistics, not just policy.
Paige Shipe
December 31, 2025 AT 18:40Let’s not pretend generics are some noble hero. Big Pharma is still making billions off them - they just license the patents to third parties who sell them at 50% markup. The system is rigged. And yes, I’ve had a generic antidepressant that made me feel like a zombie. The brand version? Life-changing. So don’t tell me they’re all the same.
Amy Cannon
January 1, 2026 AT 15:04It is, indeed, a profound and deeply concerning observation that the global pharmaceutical landscape has become increasingly stratified, with high-income nations leveraging generic substitution as a fiscal lever while low-income nations are left with no alternative but to rely upon these same generics due to systemic underfunding and structural inequities. The irony is not lost: the very mechanism that sustains healthcare access in impoverished regions is simultaneously dismissed as inferior in wealthier ones, despite identical bioequivalence standards. One must ask - is this not a moral failure encoded into policy?
Himanshu Singh
January 2, 2026 AT 06:43Man, I didn’t know generics were this important! I always thought they were just cheap stuff. But reading this made me check my last script - yep, it was generic. And I’m feelin’ fine! Maybe I should tell my doc to always go generic unless it’s something super new. Thanks for the eye-opener 😊
Greg Quinn
January 4, 2026 AT 05:29Generics are the quiet revolution nobody talks about. We celebrate AI in medicine and gene therapies, but the real unsung hero is the pill that costs 5 cents instead of $50. It’s not glamorous. It doesn’t make headlines. But it keeps people alive. And that’s the kind of progress that actually matters.
Lisa Dore
January 5, 2026 AT 18:44My mom’s on a generic statin. She used to skip doses because of the cost. Now she takes it every day. Her cholesterol’s down, her doctor’s happy, and she’s got money left for her grandkids’ birthday gifts. This isn’t just about savings - it’s about dignity. If you can afford to pay more, do it. But if you can’t? Generics aren’t a compromise - they’re justice.
Sharleen Luciano
January 7, 2026 AT 08:01How quaint. You treat generics like some moral imperative, but let’s be honest - if you’re prescribing them because you’re too lazy to understand pharmacokinetics, you’re not a hero. You’re a liability. And the fact that people celebrate this as progress? It’s a symptom of a healthcare system that’s given up on innovation and settled for survival.
Henriette Barrows
January 9, 2026 AT 04:12I used to think generics were sketchy until I got my thyroid med switched. Same pill, same results, $4 instead of $120. My doctor didn’t even mention it - I had to ask. People need to know this stuff. Don’t be shy - ask your pharmacist. They’ll tell you what’s available. Seriously, it’s that easy.
Alex Ronald
January 9, 2026 AT 06:14There’s a hidden layer here: pharmacists. In states with automatic substitution laws, they’re the frontline. They swap the brand for generic unless the script says ‘dispense as written.’ But most patients don’t know they can ask. And most pharmacists don’t proactively offer it. Training and incentives need to change. It’s not about drugs - it’s about workflow.
David Chase
January 10, 2026 AT 18:36GENERICs are why America is weak!! 🇺🇸💀 These cheap pills from China and India are flooding our system - and it’s not just about cost, it’s about NATIONAL SECURITY!! Our soldiers deserve REAL medicine, not some lab in Bangalore that probably uses rat blood as filler!! 🚨💊 #AmericaFirst #StopGenericInvasion #BrandNameOnly