Hodgkin's Disease Survival Calculator
Prognosis Calculator
Enter your disease stage and whether you have B symptoms to see estimated 5-year survival rates.
Hodgkin's disease affects the lymphatic system and is a common form of lymphoma among young adults. It’s often misunderstood, which can delay diagnosis and worsen outcomes. Below you’ll find a plain‑language guide that walks through what the disease is, why it happens, how doctors spot it, and what treatment paths look like today.
What Is Hodgkin's Disease?
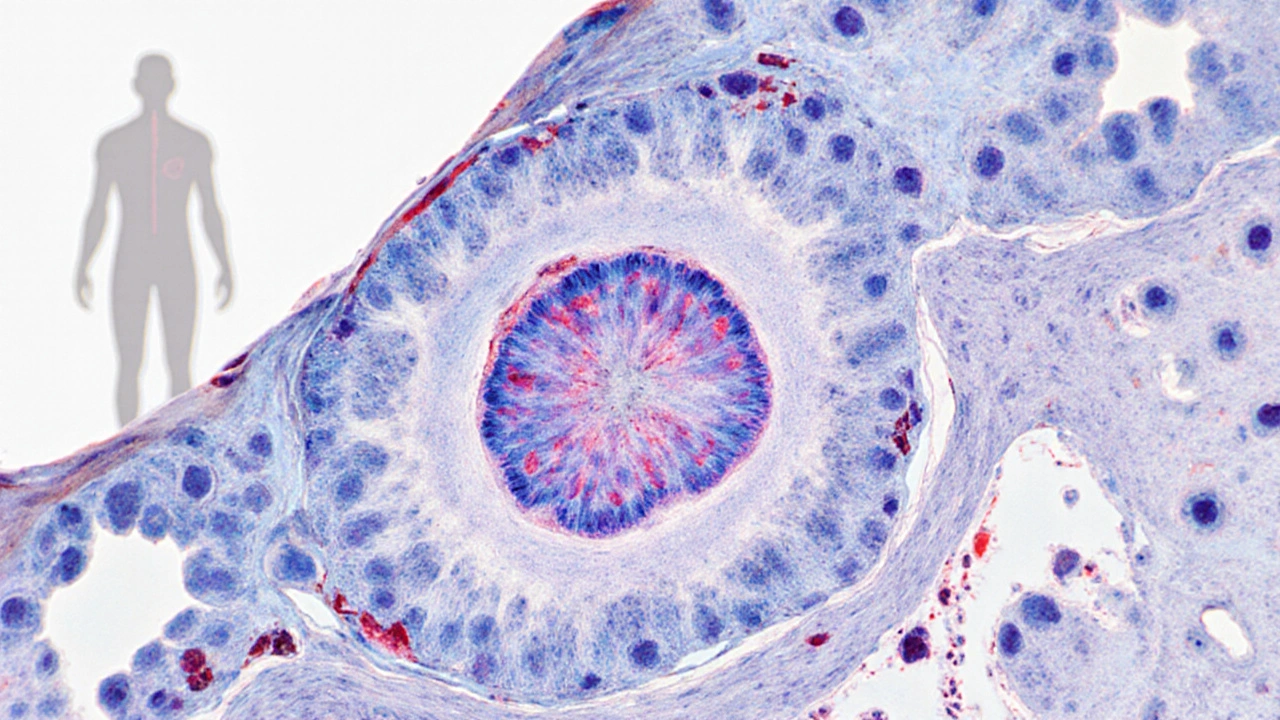
Hodgkin's disease is a type of lymphoma that starts in the lymphatic system and is distinguished by the presence of Reed‑Sternberg cells. These abnormal giant cells are the hallmark that pathologists look for under the microscope. The disease belongs to the broader family of cancers called lymphomas, but unlike non‑Hodgkin lymphomas, it follows a more predictable pattern of spread and often responds well to modern therapy.
Typical Symptoms to Watch For
Early signs can be subtle, which is why many patients mistake them for a common cold or flu. The most frequent symptom is a painless swelling of lymph nodes, especially in the neck, underarm, or groin. When other “B symptoms” appear, the suspicion should rise:
- Unexplained fever that spikes at night
- Profuse night sweats that soak clothing
- Unintended weight loss of more than 10% of body weight
- Persistent fatigue that doesn’t improve with rest
Rarely, patients experience itchy skin, coughing, or shortness of breath if the disease presses on the chest. If any of these signs linger for more than a few weeks, a medical evaluation is warranted.
Causes and Risk Factors
Unlike many solid tumors, Hodgkin's disease has no single obvious cause. Researchers have identified several risk contributors:
- Epstein‑Barr virus (EBV) infection - past infection with EBV is linked to about 30% of cases, especially in mixed‑cellularity subtypes.
- Family history - having a first‑degree relative with Hodgkin's disease roughly doubles risk.
- Immune suppression - people with HIV or those on long‑term immunosuppressive medication have higher incidence.
- Age and gender - peaks occur in early adulthood (15‑35 years) and again after age 55, with a slight male predominance.
Genetic studies suggest certain HLA‑type genes may predispose individuals, but lifestyle factors like smoking or diet have not shown a clear link.

How Doctors Diagnose the Disease
The diagnostic pathway blends clinical assessment, imaging, and tissue examination:
- Physical exam - doctors palpate enlarged nodes and note any accompanying B symptoms.
- Blood work - complete blood count and inflammatory markers help gauge overall health but cannot confirm the disease.
- Imaging - a PET/CT scan is the gold standard for staging, revealing active disease sites.
- Biopsy - an excisional node biopsy provides the tissue needed to spot Reed‑Sternberg cells. Immunohistochemistry confirms the diagnosis.
Once confirmed, the disease is staged using the AnnArbor system (StagesI‑IV) that considers the number of regions involved and the presence of B symptoms.
Staging and Prognosis
Staging determines both treatment intensity and expected outcomes. Early‑stage disease (I‑II) without B symptoms usually carries a 5‑year survival rate above 95%. Advanced stages (III‑IV) have slightly lower, yet still encouraging, survival rates around 80‑90% thanks to modern chemo‑radiotherapy protocols.
| Stage | Typical Treatment | 5‑Year Survival |
|---|---|---|
| Stage I | Combined chemo + limited radiotherapy | 96% |
| Stage II | ABVD × 4-6 cycles ± radiotherapy | 94% |
| Stage III | ABVD × 6 cycles + extended radiotherapy | 86% |
| Stage IV | BEACOPP × 6-8 cycles or modern immunotherapy | 79% |
Treatment Options
Therapy has evolved dramatically over the past two decades. The main pillars remain chemotherapy, radiotherapy, and, increasingly, targeted immunotherapy.
Standard Chemotherapy Regimens
The most widely used regimen is ABVD, which combines four drugs:
- Adriamycin (doxorubicin)
- Bleomycin
- Vinblastine
- Dacarbazine
For patients with high‑risk disease, the more intensive BEACOPP regimen is an option, though it brings greater toxicity.
| Feature | ABVD | BEACOPP |
|---|---|---|
| Drugs | Adriamycin, Bleomycin, Vinblastine, Dacarbazine | Bleomycin, Etoposide, Adriamycin, Cyclophosphamide, Vincristine, Procarbazine, Prednisone |
| Typical cycles | 4-6 | 6-8 |
| Efficacy (complete remission) | ≈85% | ≈90% |
| Major toxicities | Pulmonary (bleomycin), cardiac (doxorubicin) | Fertility loss, higher infection risk, secondary leukemias |
Radiotherapy
Low‑dose involved‑field radiotherapy (20‑30Gy) is used after chemotherapy to mop up residual disease, especially in early‑stage cases. Modern planning techniques (IMRT) limit exposure to heart, lungs, and breast tissue.
Immunotherapy and Targeted Agents
Checkpoint inhibitors such as nivolumab and pembrolizumab, which block the PD‑1 pathway, have shown high response rates in relapsed or refractory Hodgkin's disease. They are often combined with reduced‑dose chemo to spare patients from cumulative toxicity.
Clinical Trials and Emerging Approaches
Ongoing studies explore CAR‑T cell therapy directed at CD30, antibody‑drug conjugates, and novel Bruton’s tyrosine kinase inhibitors. Participation in a trial can provide access to cutting‑edge treatment while contributing to scientific progress.

Managing Side Effects and Follow‑Up Care
Even with curative intent, treatment leaves a trail of short‑ and long‑term effects. Common acute issues include nausea, fatigue, and low blood counts. Supportive measures-anti‑emetics, growth‑factor support, and nutritional counseling-help keep patients on track.
Long‑term surveillance focuses on:
- Secondary cancers (breast, lung, thyroid) - annual imaging as recommended
- Cardiac health - echocardiograms every 2-3years for patients exposed to anthracyclines
- Infertility - sperm banking or ovarian tissue preservation before treatment
- Psychosocial well‑being - counseling, support groups, and survivorship programs
Most survivors return to normal life within 1-2years, but lifelong follow‑up with an oncologist is essential to catch late effects early.
Key Takeaways
- Hodgkin's disease is a lymphoma marked by Reed‑Sternberg cells; early detection greatly improves cure rates.
- Typical signs are painless lymph node swelling plus B symptoms (fever, night sweats, weight loss).
- Risk factors include prior EBV infection, family history, and immune suppression.
- Diagnosis requires a biopsy and PET/CT for accurate staging.
- First‑line treatment usually involves ABVD chemo±radiotherapy; high‑risk cases may receive BEACOPP or immunotherapy.
- Survivors need lifelong monitoring for secondary cancers and organ toxicity.
Frequently Asked Questions
Can Hodgkin's disease be cured?
Yes. With modern chemo‑radiotherapy protocols, about 85‑95% of patients achieve long‑term remission, especially when the disease is caught early.
What makes Hodgkin's disease different from non‑Hodgkin lymphoma?
The presence of Reed‑Sternberg cells is the defining feature. Hodgkin's also spreads in a predictable, step‑wise pattern and often responds better to standard chemotherapy.
Is there a genetic test for Hodgkin's disease?
No single genetic test exists. Researchers have identified certain HLA‑type markers that raise risk, but routine screening isn’t recommended.
How long does treatment usually last?
Chemotherapy courses typically run 4-6 months, with radiotherapy given over 2-4 weeks afterward. Follow‑up visits continue for several years.
Can children get Hodgkin's disease?
Yes, although it’s less common. Pediatric protocols often use lower‑dose chemo to reduce long‑term side effects while preserving high cure rates.
What lifestyle changes help during treatment?
Maintain a balanced diet rich in protein, stay hydrated, and get gentle exercise as tolerated. Avoid smoking, which can worsen lung toxicity from bleomycin.

Carl Mitchel
October 14, 2025 AT 16:24While many readers skim over oncology articles, it's essential to grasp the gravity of Hodgkin's disease and the responsibility each of us bears to stay informed. The detailed breakdown of symptoms and staging underscores how early detection can be a matter of life or death. Ignoring the B symptoms or dismissing the risk factors is not just careless, it's morally indefensible. A well‑rounded understanding empowers patients to demand appropriate care and pushes the medical community toward better outcomes. Knowledge, after all, is a civic duty.
Suzette Muller
October 15, 2025 AT 22:53Thank you for sharing such a clear overview; the empathy woven through the description of B symptoms really resonates. Patients often feel isolated when night sweats and weight loss become daily burdens, so highlighting these signs early can save precious time. The treatment section wisely balances optimism with realistic expectations about side effects. Please keep providing these compassionate resources-they make a tangible difference.
Josh SEBRING
October 17, 2025 AT 05:22Honestly, this whole survival calculator feels like a gimmick when real lives are at stake. People can’t reduce complex oncology to a percent on a web page.
Lily Tung
October 18, 2025 AT 11:51One must begin by acknowledging the historical lineage of Hodgkin's disease scholarship which has been meticulously chronicled over the past century. The identification of Reed‑Sternberg cells marked a paradigm shift in hematopathology thereby granting clinicians a definitive diagnostic hallmark. Subsequent elucidation of the Ann Arbor staging system provided a structured framework for therapeutic stratification. Contemporary therapeutic regimens such as ABVD have demonstrated remarkable efficacy as evidenced by longitudinal cohort studies. Nevertheless the specter of long‑term cardiopulmonary toxicity persists necessitating vigilant surveillance. The incorporation of PET‑CT imaging has refined response assessment and facilitated de‑escalation strategies in select populations. Moreover the advent of checkpoint inhibition has opened new avenues for refractory disease management. It is imperative to contextualize survival statistics within the broader epidemiological landscape. The reported five‑year survival rates surpass ninety percent for early stage disease fostering a sense of cautious optimism. Conversely advanced stage disease continues to challenge oncologists despite incremental gains in overall survival. Ongoing clinical trials exploring CD30‑targeted CAR‑T cell therapy exemplify the relentless pursuit of curative intent. Ethical considerations surrounding treatment intensity versus quality of life remain paramount. Multidisciplinary survivorship programs have emerged to address secondary malignancies and psychosocial well‑being. Patient advocacy groups play a vital role in disseminating education and fostering community support. In sum the trajectory of Hodgkin's disease management reflects both scientific rigor and compassionate care.
Melissa Gerard
October 19, 2025 AT 18:20Just another article with the same old stats 🙄.
Manju priya
October 21, 2025 AT 00:48Your dedication to demystifying Hodgkin's disease will undoubtedly empower countless patients; keep shining this beacon of hope 😊.
Jeff Bellingham
October 22, 2025 AT 07:17While the article presents a comprehensive overview, it would benefit from a more nuanced discussion of long‑term survivorship issues, particularly regarding secondary malignancies and cardiac monitoring protocols.
Matthew Balbuena
October 23, 2025 AT 13:46Yo, that rundown on the chemo combos is solid but don’t forget to watch out for those nasty lung vibes from bleomycin – stay sharp and keep hustlin’!
Bansari Patel
October 24, 2025 AT 20:15If we continue to treat cancer as merely a biological glitch instead of confronting the existential dread it imposes, we betray our own humanity and fuel a cycle of complacent denial.
Rebecca Fuentes
October 26, 2025 AT 02:44The article admirably balances scientific rigor with accessible language, thereby serving as an invaluable resource for both clinicians and patients navigating the complexities of Hodgkin's disease.
Jacqueline D Greenberg
October 27, 2025 AT 08:12Hey folks, great post! Super helpful and easy to read – thanks for breaking it down for all of us.