What Are De Facto Combinations?
De facto combinations happen when a patient takes two or more separate generic pills instead of one fixed-dose combination (FDC) tablet that contains the same drugs. For example, instead of taking a single pill with amlodipine and valsartan for high blood pressure, they take one blue pill of amlodipine and one white pill of valsartan. This isn’t an approved product-it’s a workaround. But it’s common. In fact, nearly half of all hypertension patients on combination therapy in the U.S. get their meds this way, according to IQVIA data from 2022.
Why does this happen? It’s not random. Doctors do it for real reasons: cost, flexibility, and sometimes because the FDC doesn’t offer the right dose. But there’s a hidden cost. These unapproved mixes skip the safety checks that FDCs go through. No one tested whether these two generics work well together in the body. No one studied if they break down the same way in your stomach. That’s not just theoretical-it’s risky.
Why Doctors Choose Separate Generics
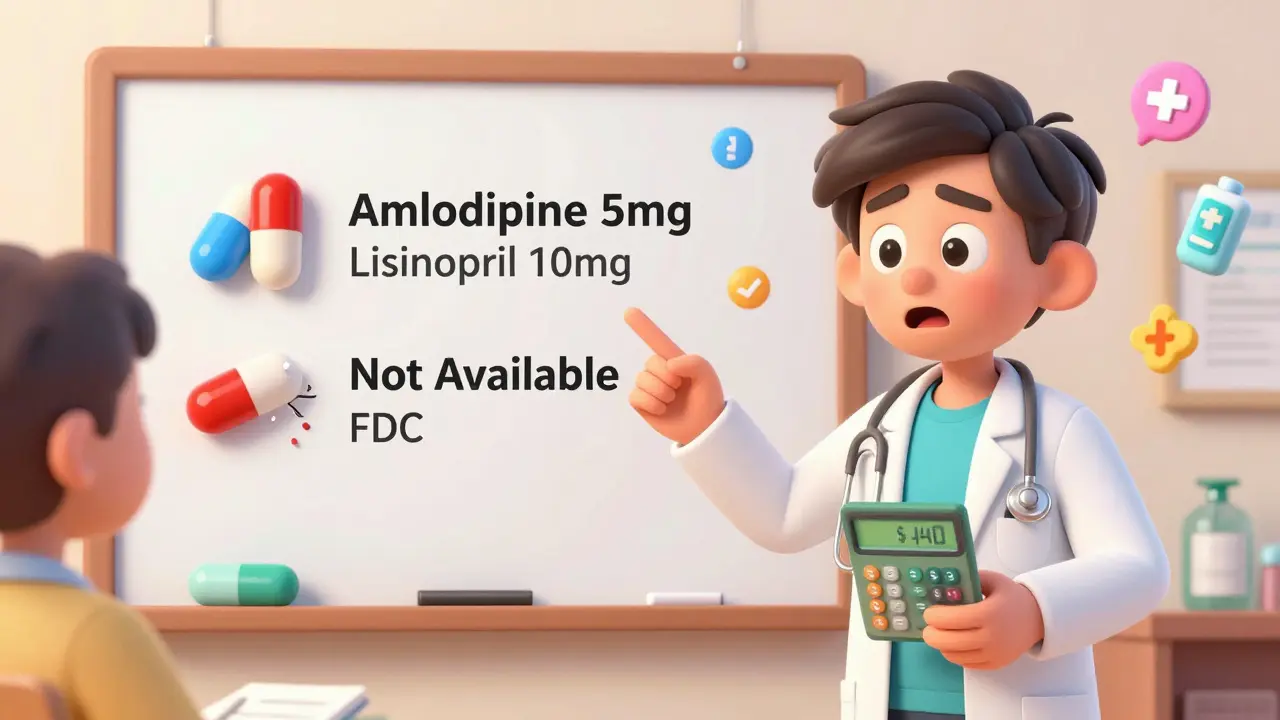
Let’s say you have high blood pressure. Your doctor wants to combine two drugs: amlodipine and lisinopril. The only FDC available comes in 10mg/20mg. But your body needs 5mg of amlodipine and 10mg of lisinopril. There’s no FDC for that. So your doctor writes two prescriptions. That’s de facto combination therapy in action.
This isn’t rare. In diabetes, 67% of patients need individualized dosing, and most FDCs don’t offer that precision, per the American Diabetes Association’s 2022 guidelines. Same with kidney disease. If your kidneys can’t handle a full dose of one drug, you can’t use a standard FDC-you need to cut the dose of just one component. Separate generics make that possible.
Cost is another driver. In India, a 2012 parliamentary report found many FDCs offered no real benefit over individual drugs-and were often more expensive. Even in the U.S., if your insurance doesn’t cover the branded FDC but covers both generics at $5 each, it’s cheaper than a $40 FDC. Some patients save $15 a month by splitting the pills. That matters when you’re paying out of pocket.
The Hidden Risks of Mixing Pills
Here’s the problem: when you take two separate pills, you’re assuming they’ll behave the same way as if they were in one tablet. But that’s not guaranteed. FDCs are tested together. The manufacturers check if the drugs interact chemically. Do they degrade each other? Do they affect how each is absorbed? Is the coating compatible? All of that is studied before the FDC hits the market.
De facto combinations skip that. You might be taking two FDA-approved generics-but never tested together. A 2020 FDA review found that 12.7% of generic drugs had clinically meaningful differences in how they released into the bloodstream compared to the brand. That means one generic might release faster than another. If you’re taking them separately, you could get a spike in one drug and a delay in the other. That’s not just inconvenient-it could cause side effects or reduce effectiveness.
And what about drug interactions? FDCs must prove they’re safer than using the drugs alone. That’s not required for de facto combinations. There’s no data on whether your two generics increase the risk of low blood pressure, kidney stress, or dizziness when taken together. You’re flying blind.
Pill Burden and Adherence: The Silent Killer
One of the biggest reasons FDCs were invented was to make it easier for people to take their meds. Take one pill instead of three. That’s simple. But when you switch from an FDC to separate generics, you’re adding pills. And every extra pill lowers your chance of sticking with the regimen.
Studies show each additional pill reduces adherence by about 16%. A 2023 study in PubMed found patients on FDCs had 22% higher adherence than those on the same drugs taken separately. That’s huge. Missed doses mean higher blood pressure, higher A1c, higher risk of stroke or heart attack.
Patients know this. On PatientsLikeMe, 63% of people on separate generics said they struggled to remember which pill to take when. On Reddit, one user wrote: “I switched from a single Amlodipine/Benazepril pill to two separate ones to save $15 a month. I missed doses twice because I forgot which blue pill was which.”
It’s not just about forgetting. It’s about confusion. A 2022 survey of 1,532 pharmacists found 72% worried about medication errors with de facto combinations. Color-coding helps, but it’s not foolproof. And not everyone has access to a pharmacy that offers that service.
When De Facto Combinations Make Sense
Let’s be clear: this isn’t always a bad idea. Sometimes, it’s the only smart choice.
Take HIV treatment. Most patients use FDCs because adherence is life-or-death. But in oncology or complex kidney disease, where dosing needs to change weekly or monthly, FDCs are too rigid. A 2023 physician on Student Doctor Network said: “I prescribe separate generics for HIV patients who need dose adjustments-but I always give them a color-coded schedule. It’s extra work, but it saves lives.”
Another example: a diabetic with kidney impairment. Their doctor can’t use a standard FDC because one drug needs to be lowered. Separate generics let them fine-tune. One patient on Drugs.com gave a 5-star review: “I’m on separate Metformin and Sitagliptin because the FDC dose was too strong for my kidneys. My A1c’s been 6.2% for 18 months.”
So it’s not about banning de facto combinations. It’s about using them wisely-only when needed, and only with support.

How to Stay Safe If You’re on Separate Generics
If you’re taking separate pills instead of an FDC, here’s how to protect yourself:
- Use a pill organizer. Color-coded trays or apps like Medisafe can help you track what to take and when.
- Ask for synchronized refills. Make sure all your pills are due on the same day. No one should be running out of one drug while another is full.
- Get a medication review. Every six months, ask your pharmacist to check your entire list. They can spot interactions you might miss.
- Know your doses. Don’t just remember “the blue pill.” Know the name and milligram amount of each one. Write it down.
- Ask if an FDC exists. Sometimes a new FDC with your exact dose was approved last year. Ask your doctor to check.
Some pharmacies, like PillPack by Amazon, now offer personalized packaging for complex regimens. They sort your pills by time of day and send them in labeled pouches. Patients using this service saw a 41% drop in missed doses, according to their 2021 report.
The Future: Smarter FDCs, Not Just More Pills
The industry is starting to respond. AstraZeneca filed a patent in 2022 for a modular FDC that lets you swap out doses without changing the whole tablet. Think of it like LEGO-same base, different inserts. That could solve the flexibility problem without going back to separate pills.
The FDA is also watching. In January 2023, they issued a safety alert after 147 adverse events were linked to untested combinations. They’re pushing for better tracking and prescribing rules.
Meanwhile, the EMA is running a multi-year study to understand how often de facto combinations cause harm. Results are expected by late 2024.
One thing’s clear: the future won’t be all FDCs or all separate generics. It’ll be smarter prescribing. Doctors who know when to use each. Pharmacies that support complex regimens. Patients who understand why it matters.
Final Thought: Flexibility Isn’t Free
Choosing separate generics might save you money today. But if you miss doses, end up in the ER, or have a stroke because your blood pressure wasn’t controlled, the cost skyrockets. De facto combinations aren’t inherently wrong-but they’re not risk-free either. They require more attention, more support, and more responsibility from everyone involved.
The goal isn’t to eliminate them. It’s to make sure they’re used only when necessary-and with eyes wide open.


Jason Shriner
January 11, 2026 AT 06:32Jennifer Littler
January 12, 2026 AT 03:44Alfred Schmidt
January 13, 2026 AT 15:30Alex Smith
January 15, 2026 AT 09:14Roshan Joy
January 15, 2026 AT 20:18Adewumi Gbotemi
January 16, 2026 AT 22:36Michael Patterson
January 17, 2026 AT 05:36Madhav Malhotra
January 17, 2026 AT 19:51Priya Patel
January 18, 2026 AT 00:47