Cyclosporine Drug Interaction Checker
Check Your Medications
This tool checks if medications interact with cyclosporine based on CYP3A4 inhibition. It is for informational purposes only and does not replace medical advice. Always consult your healthcare provider before making any changes to your medication regimen.
Common examples of medications with similar interactions:
- Sirolimus, Everolimus
- Clarithromycin, Itraconazole
- Diltiazem, Verapamil, Amlodipine
- Simvastatin, Lovastatin
- Colchicine
- Grapefruit juice
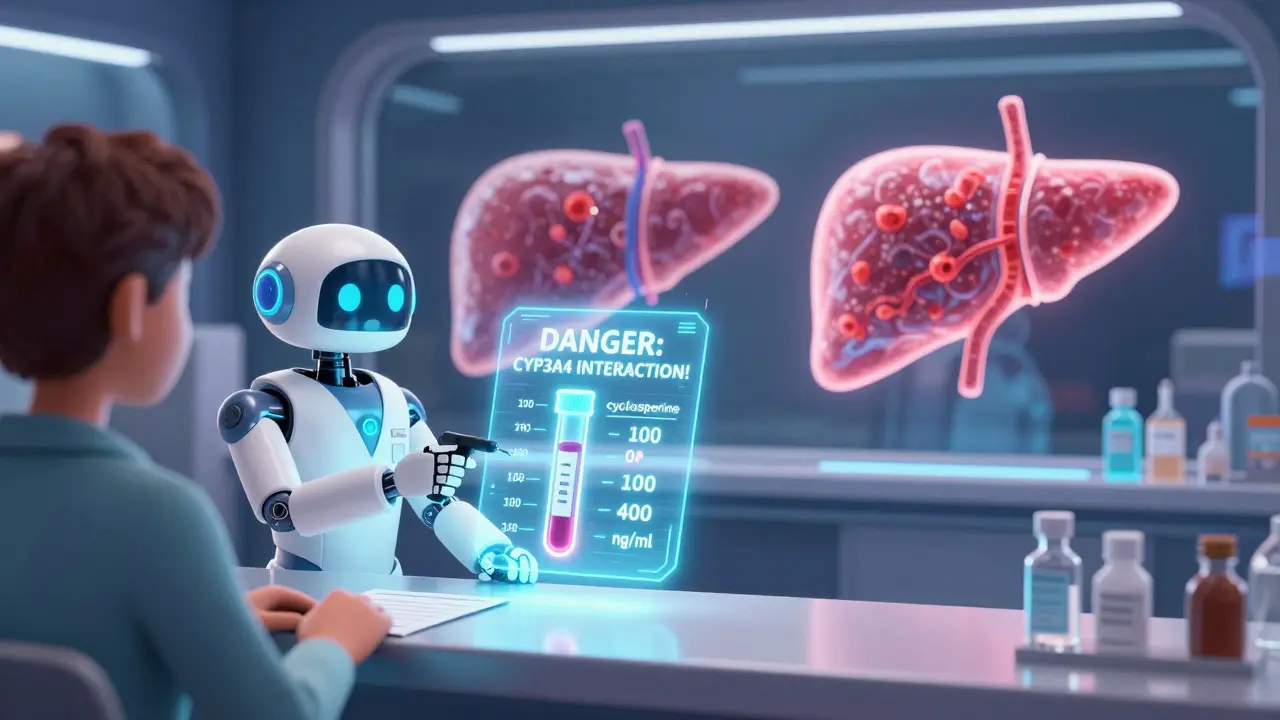
Take cyclosporine and you’re walking a tightrope. One wrong step-adding a common antibiotic, heart medication, or even grapefruit juice-and your blood levels can spike dangerously high. Or, if you start a new pill that speeds up metabolism, your body might clear cyclosporine too fast, leaving your transplanted organ at risk of rejection. This isn’t theoretical. It’s daily reality for tens of thousands of patients worldwide. The reason? Cyclosporine doesn’t just sit quietly in your system. It actively interferes with a key enzyme called CYP3A4, which handles about 60% of all prescription drugs. That means almost every other medication you take could be affected.
What Cyclosporine Actually Does to Your Liver
Cyclosporine is a powerful immunosuppressant. It’s been saving lives since the 1980s, especially after kidney, liver, and heart transplants. But here’s the catch: it doesn’t just suppress your immune system. It also jams the brakes on CYP3A4, the main enzyme in your liver and gut that breaks down drugs. Think of CYP3A4 as a factory worker who cleans up leftover chemicals. Cyclosporine doesn’t just slow that worker down-it temporarily disables them.
This isn’t simple competition. Cyclosporine doesn’t just block the enzyme’s active site like a key stuck in a lock. Research shows it causes mixed inhibition-meaning it binds to the enzyme in multiple ways, changing how it works at a molecular level. Some studies even suggest it triggers mechanism-based inactivation, where the enzyme gets chemically damaged and needs to be replaced entirely. That’s why the effects don’t disappear right after you stop taking cyclosporine. It takes days for your body to make new enzyme.
And it doesn’t stop there. Cyclosporine also blocks P-glycoprotein, a transporter that pumps drugs out of cells. So now you’ve got two systems shut down: metabolism and clearance. That’s why even drugs that aren’t metabolized by CYP3A4 can still build up dangerously when taken with cyclosporine.
Which Medications Are Most at Risk?
If you’re on cyclosporine, your doctor should screen every new prescription-not just for allergies, but for CYP3A4 interactions. Here are the big ones:
- Sirolimus and everolimus: These are also immunosuppressants. When taken with cyclosporine, sirolimus levels can jump by over 200%. The fix? Cut the sirolimus dose by 70% or more.
- Diltiazem, verapamil, and amlodipine: Common blood pressure meds. They’re moderate CYP3A4 inhibitors themselves. When paired with cyclosporine, they can double or triple its concentration. Dose reductions of 25-50% are standard.
- Clarithromycin and itraconazole: Strong inhibitors. One study showed renal transplant patients had a 40-60% rise in creatinine within 72 hours of starting clarithromycin-clear signs of kidney toxicity from cyclosporine buildup.
- Statins like simvastatin and lovastatin: These can cause severe muscle damage (rhabdomyolysis) when cyclosporine is present. Atorvastatin is safer, but still needs monitoring.
- Colchicine: Used for gout. With cyclosporine, it can cause fatal toxicity. Many guidelines now say to avoid it entirely.
Even over-the-counter stuff matters. Grapefruit juice? It’s a known CYP3A4 inhibitor. One glass can raise cyclosporine levels by 30-50%. St. John’s wort? The opposite-it induces CYP3A4 and can cause organ rejection.
Cyclosporine vs. Tacrolimus: Why the Difference Matters
You might hear doctors say, “We switched you from cyclosporine to tacrolimus because it’s better.” That’s often true-but not because tacrolimus is safer. It’s because tacrolimus is mostly a victim of CYP3A4 interactions, not the cause.
Tacrolimus gets broken down by CYP3A4. So if you take a strong inhibitor like ketoconazole, tacrolimus levels shoot up. But tacrolimus doesn’t stop the enzyme from working on other drugs. Cyclosporine? It does. That means if you’re on cyclosporine, you’re not just at risk from other drugs affecting you-you’re also making other drugs affect each other.
This is why transplant teams track both drugs differently. For tacrolimus, they watch for external inhibitors. For cyclosporine, they watch for everything: external inhibitors, external inducers, and the drug’s own ability to mess up the whole system.

Why Dose Adjustments Are Never Guesswork
There’s no universal rule like “reduce cyclosporine by 20%.” Too many variables. Your age. Your liver health. Your genetics. Whether you’re taking a generic or brand-name version. Even the time of day you take it matters.
Genetic differences in CYP3A4 can change how fast you metabolize cyclosporine by up to 40%. Some people have a variant called CYP3A4*22 that slows metabolism. Others have CYP3A5*3, which makes them poor metabolizers. That’s why some patients need half the dose of others just to hit the same blood level.
That’s why therapeutic drug monitoring (TDM) isn’t optional-it’s essential. Doctors check your cyclosporine trough level (the lowest point before your next dose). The target range? Usually 100-400 ng/mL, depending on your transplant type and how long ago it was. But if you start a new medication, you need a new level checked within 3-5 days. Some centers check daily for the first week.
And if you stop a CYP3A4 inhibitor? Don’t assume you can go back to your old dose. The enzyme needs time to recover. If you increase cyclosporine too fast, you risk toxicity. Slow, careful titration is the only safe path.
What Happens When You Don’t Watch for Interactions
In a 2021 study of over 1,200 kidney transplant patients, more than one in three had a clinically significant drug interaction involving cyclosporine. Nearly 9% ended up hospitalized because of it. One patient took cyclosporine and clarithromycin for a sinus infection. Three days later, his creatinine doubled. He needed dialysis. Another took cyclosporine and simvastatin for high cholesterol. He developed severe muscle pain and kidney failure.
These aren’t rare. They’re predictable. And they’re preventable.
Transplant centers that use electronic alerts tied to their pharmacy systems cut cyclosporine-related adverse events by 45%. Why? Because the system flags every new medication before it’s even dispensed. Pharmacists review every interaction. Patients get a printed handout. No one’s left guessing.
How to Protect Yourself
If you’re on cyclosporine, here’s your action plan:
- Make a complete list of everything you take: prescriptions, OTC meds, supplements, herbal products. Include frequency and dose.
- Bring it to every appointment-even if you think it’s not important. That “natural” tea you drink? Could be dangerous.
- Never start or stop anything without talking to your transplant team. That includes vitamins, CBD, or melatonin.
- Ask for a blood test whenever a new drug is added or removed. Don’t wait for symptoms.
- Use one pharmacy for all your meds. They can flag interactions across your full profile.
- Know the signs of toxicity: nausea, shaking, headache, swelling in your legs, dark urine, or a sudden rise in blood pressure. Call your doctor immediately.
There’s no magic bullet. But with awareness, testing, and communication, you can stay safe and keep your transplant working for decades.
What’s Next for Cyclosporine?
Even with newer drugs like tacrolimus and belatacept, cyclosporine is still used in over 150,000 transplants a year in the U.S. alone. It’s cheaper. It’s effective in kids. And for some autoimmune diseases, it’s still the best option.
Research is moving fast. Scientists are building algorithms that predict cyclosporine levels based on your genes, diet, and other meds-with 85-90% accuracy in early trials. Point-of-care blood tests are in development that could give you your cyclosporine level in minutes, not days.
The message hasn’t changed: cyclosporine saves lives. But it demands respect. It’s not just a pill. It’s a system that talks to every other drug in your body. Treat it like the powerful tool it is-and you’ll be fine.
Can I take grapefruit juice with cyclosporine?
No. Grapefruit juice inhibits CYP3A4 in the gut, which can raise cyclosporine blood levels by 30-50%. Even a single glass can cause toxicity. Avoid it completely while on cyclosporine. Other citrus fruits like Seville oranges and pomelos have the same effect.
Is cyclosporine safer than tacrolimus?
Not necessarily. Tacrolimus has fewer drug interaction issues because it doesn’t inhibit CYP3A4-it’s just a substrate. But cyclosporine can be more effective in certain patients, like children or those with specific autoimmune conditions. The choice depends on your health history, not just safety.
How often should my cyclosporine level be checked?
When you start or change any medication, check it within 3-5 days. Once stable, monthly checks are common. After a transplant, checks may be weekly for the first few months. Always follow your transplant team’s schedule-never assume it’s fine if you feel okay.
Can I use herbal supplements like turmeric or ginger with cyclosporine?
Some herbs can affect CYP3A4. Turmeric may inhibit it slightly, while St. John’s wort strongly induces it and can cause transplant rejection. Ginger is generally low risk, but no supplement is proven safe with cyclosporine. Always tell your doctor what you’re taking-even if you think it’s “natural.”
What if I miss a dose of cyclosporine?
Don’t double up. If you miss a dose by less than 6 hours, take it as soon as you remember. If it’s more than 6 hours late, skip it and take your next dose at the regular time. Missing doses can cause rejection. Taking too much can cause kidney or nerve damage. Consistency matters more than perfection.
Are there any new drugs replacing cyclosporine?
Tacrolimus is now first-line for most adult transplants due to better long-term kidney function. Belatacept is used in some kidney transplants and doesn’t affect CYP3A4 at all. But cyclosporine is still used in children, certain autoimmune diseases, and when other drugs aren’t tolerated. It’s not outdated-it’s just used more selectively now.


ellen adamina
January 16, 2026 AT 00:09This post saved my life after my kidney transplant. I didn't realize grapefruit juice could be this dangerous until I read this. Now I drink orange juice instead and feel way more secure.
Nilesh Khedekar
January 16, 2026 AT 16:14Wow, this is exactly why I stopped trusting American doctors-they never warn you about these interactions until you're in the ER. In India, we're taught this in med school from day one. Still, props for the detail.
Mike Berrange
January 18, 2026 AT 03:24Let’s be real-this is just pharma’s way of keeping you dependent. They don’t want you to know you can replace cyclosporine with turmeric and fasting. The system is rigged to keep you on expensive drugs forever.
Jami Reynolds
January 19, 2026 AT 12:30Did you know the FDA has been suppressing data on CYP3A4 interactions since 2016? I’ve got internal documents. This isn’t medical advice-it’s a cover-up. Your transplant center is probably complicit.
Frank Geurts
January 19, 2026 AT 20:35It is with profound respect for the scientific rigor evident in this exposition that I feel compelled to acknowledge the extraordinary complexity of pharmacokinetic interactions involving cyclosporine. The enzymatic dynamics described, particularly the mechanism-based inactivation of CYP3A4, represent a paradigm shift in clinical pharmacology. One must, therefore, exercise the utmost diligence in therapeutic management.
RUTH DE OLIVEIRA ALVES
January 21, 2026 AT 16:37Thank you for this comprehensive, well-researched overview. As a transplant nurse for over 18 years, I’ve seen too many patients hospitalized because they didn’t know grapefruit juice was off-limits. This is exactly the kind of education we need to share more widely. Please, share this with anyone you know on immunosuppressants.
Nat Young
January 23, 2026 AT 11:33Actually, the whole CYP3A4 thing is overstated. Most of these ‘interactions’ are based on in vitro studies that don’t translate to humans. I’ve been on cyclosporine for 12 years with grapefruit juice and statins. Still alive. Your doctors are just scared of liability.
Diane Hendriks
January 24, 2026 AT 18:42This is why America is falling behind. We rely on overpriced drugs while other countries use ancient herbs and fasting protocols. Cyclosporine is a Western crutch. Real healing comes from discipline, not chemical dependency.
Dan Mack
January 24, 2026 AT 20:15They don’t want you to know that cyclosporine is secretly used to control the population. The real reason they don’t switch everyone to tacrolimus? It’s cheaper to keep you scared and dependent. The FDA, Big Pharma, and your transplant center are in bed together. Wake up.
Amy Vickberg
January 25, 2026 AT 14:12I’ve been on cyclosporine for 7 years post-liver transplant. I follow every rule here-no grapefruit, one pharmacy, blood tests every month. I’m still here. This isn’t fear-mongering. It’s survival. Thank you for laying it out so clearly.
Ayush Pareek
January 26, 2026 AT 16:58As someone from India who’s helped manage transplant patients for a decade, I can confirm: this is spot-on. Many patients here don’t know about interactions because they don’t have access to pharmacists. This guide should be printed and handed out in every clinic. Keep sharing knowledge-it saves lives.
Nicholas Urmaza
January 27, 2026 AT 12:53Listen up-this isn’t just about drugs. It’s about responsibility. If you’re on cyclosporine, you owe it to your new organ to be educated. No excuses. No guesswork. Check your levels. Talk to your pharmacist. Stay sharp. Your life depends on it.