Medical Research: Genetics and Scar Healing
Genetics shape how we heal and how scars form. If you've ever wondered why a small cut left a faint line while a friend ended up with a thick raised scar, genes are part of the answer. This page explains what researchers have found and what it means for everyday wound care.
How genes affect scarring
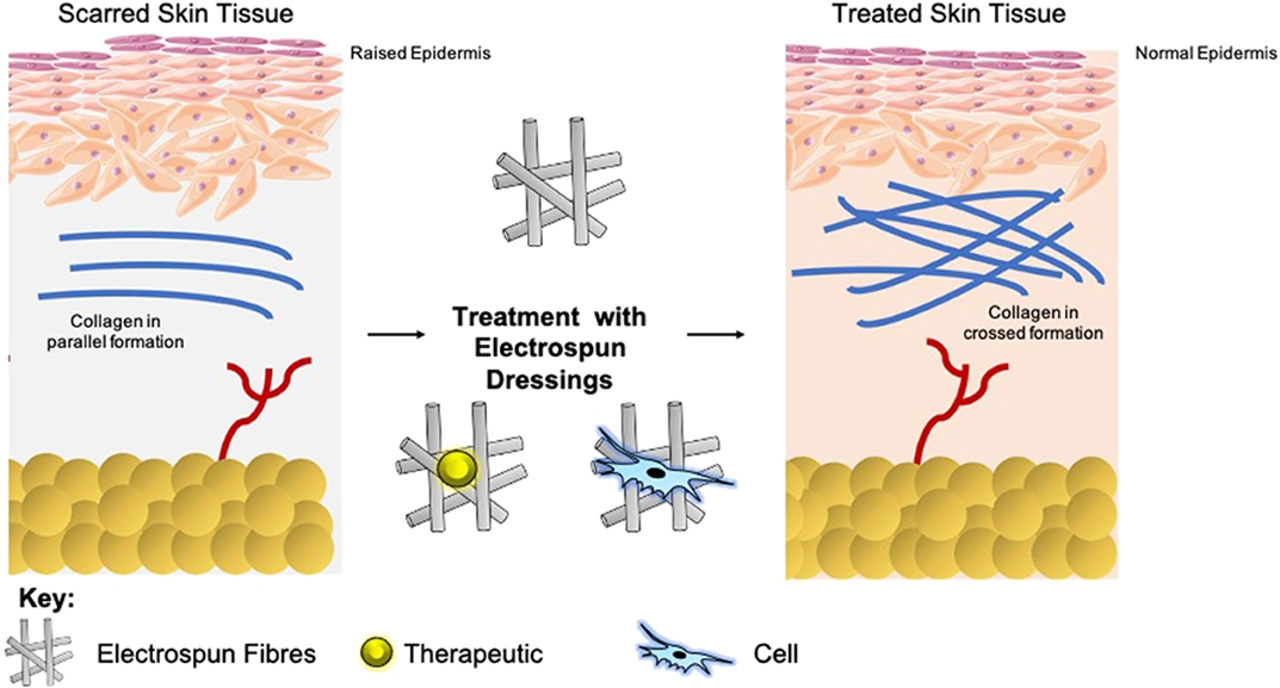
Researchers have identified specific genes that influence inflammation, collagen production, and skin cell behavior after injury. Variants in genes like TGF-β, COL1A1, and MMPs can change how much scar tissue builds and whether healing is fast or slow. For example, higher TGF-β activity is linked to thicker, raised scars (hypertrophic scars and keloids). That doesn't mean your fate is fixed; environment and treatment also matter.
Why this matters for you
Understanding genetic risks helps tailor treatments. If someone has a family history of keloids, doctors may recommend gentler wound care, early silicone sheets, or steroid options after surgery. New research is exploring gene-targeted therapies and drugs that adjust scarring pathways. Some clinical trials show promising results, but most treatments are still in testing phases.
Practical tips from research
- Treat wounds promptly: clean, gentle pressure, and proper dressings reduce infection and excessive inflammation.
- Protect from sun: UV exposure can darken scars and worsen appearance.
- Use silicone sheets or gels: evidence supports silicone for flattening and softening scars when used consistently.
- See a clinician early for abnormal scarring: early steroid injections or laser treatments work better than late interventions.
What the studies are saying
A recent clinical review compared standard care to strategies that target fibrosis pathways and found reduced scar thickness in groups that received early intervention. Another study tracked families prone to keloids and confirmed a hereditary pattern linked to several gene variants. These studies suggest a mix of genetics and lifestyle determines outcomes.
How we can use this now
Ask your provider about your personal and family healing history before surgery or if you have recurrent problematic scars. Simple steps like silicone application and sun protection are low-risk and can help. If scarring is severe, referral to a dermatologist or plastic surgeon can open options like injections, lasers, or clinical trials.
Questions to ask your clinician: Do I have a family history of keloids? Are there topical or injection options to reduce risk after surgery? Is there a referral for genetic counseling or clinical trials? Keep photos of healing progress for follow up. If you plan cosmetic procedures, mention past scar behavior—surgeons can adjust techniques to lower risk. Finally, think about timing: many interventions are more effective when started within weeks after injury. That short window makes early conversations and follow up useful.
If you want, bookmark this page and check back—new studies and practical tips get added regularly.