Workplace Antihistamine Safety Checker
Check if your antihistamine is safe for safety-sensitive jobs. Many people don't realize first-generation antihistamines can impair your ability to work safely even when you don't feel sleepy.
Enter your antihistamine name to see if it's safe for work
Many people take antihistamines without thinking twice-especially during allergy season. But what if that little pill is quietly making you unsafe at work? If you drive, operate machinery, or work in construction, healthcare, or transportation, the answer might be yes. First-generation antihistamines like diphenhydramine (Benadryl), chlorpheniramine, and hydroxyzine don’t just stop sneezing-they slow down your brain. And you might not even realize it.
Why You Don’t Feel Drowsy But Still Can’t Focus
One of the most dangerous myths about sedating antihistamines is that if you don’t feel sleepy, you’re fine. That’s not true. Studies show people often report feeling alert while their reaction time drops by 25-30% and their ability to stay in their lane on the road declines by 50%. This gap between how you feel and how your brain is actually performing is called impaired awareness. It’s why truck drivers fail roadside cognitive tests after taking Benadryl-even though they swear they’re wide awake.
The reason? These drugs cross the blood-brain barrier easily. Histamine in your brain helps keep you alert. When antihistamines block it, your brain’s natural wakefulness signal gets turned down. You might yawn once or twice, but your body doesn’t scream ‘danger’ like it would after a sleepless night. Instead, your focus, judgment, and coordination quietly degrade. By the time you notice something’s off, it’s often too late.
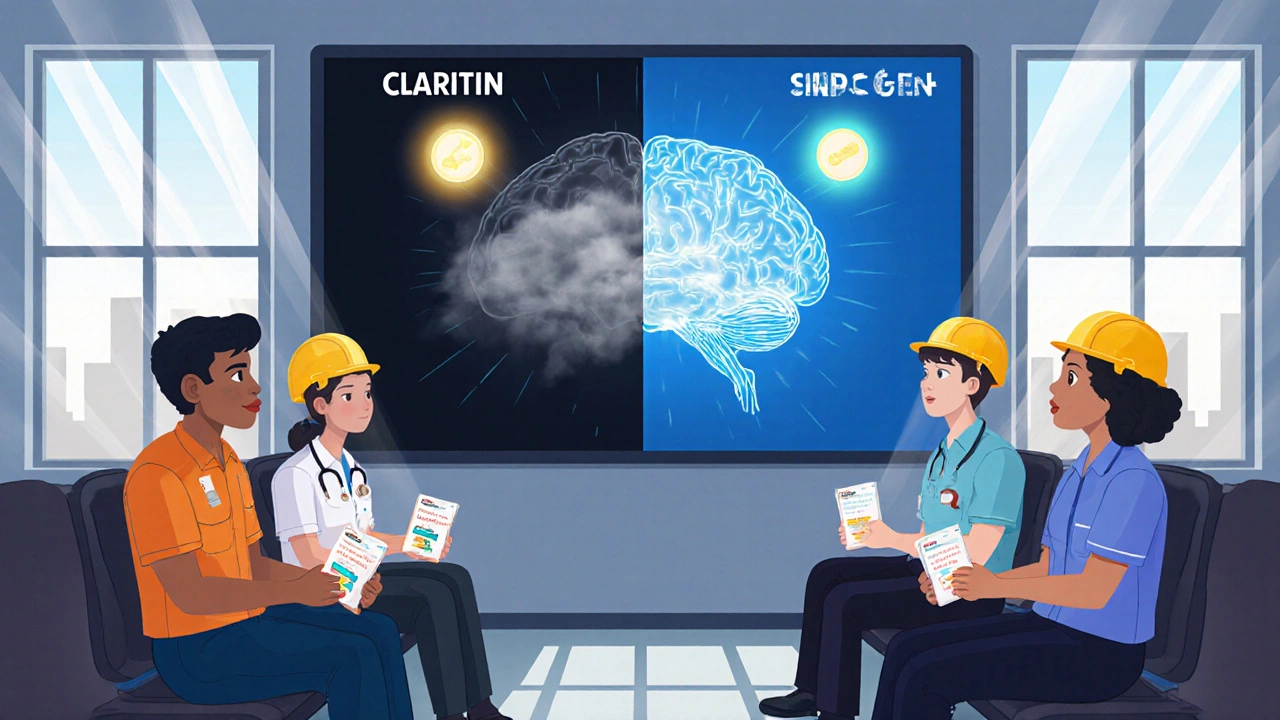
First-Generation vs. Second-Generation: The Safety Divide
Not all antihistamines are created equal. There’s a clear split between the old and the new.
First-generation antihistamines-like Benadryl, Chlor-Trimeton, and Vistaril-are cheap, widely available, and effective for allergies. But they’re also the most dangerous for workers. They linger in your system for 15 to 30 hours. Even if you take one at night, you could still be impaired the next day. And if you take more than one dose? The effects pile up. Combine them with alcohol, painkillers, or even some cold meds, and the risk multiplies.
Second-generation antihistamines-loratadine (Claritin), cetirizine (Zyrtec), fexofenadine (Allegra), and newer ones like bilastine-were designed to avoid this. Their chemical structure makes them less likely to enter the brain. They’re pumped out by a protein called P-glycoprotein, acting like a bouncer keeping them away from your central nervous system. In driving simulators, these drugs perform almost identically to a placebo. A 2013 study found no significant impairment in reaction time or coordination, even at double the recommended dose.
Here’s the real-world difference:
| Feature | First-Generation (e.g., Benadryl) | Second-Generation (e.g., Claritin, Allegra) |
|---|---|---|
| Brain penetration | High-easily crosses blood-brain barrier | Low-blocked by P-glycoprotein |
| Half-life | 15-30 hours | 8-12 hours |
| Impairment in driving tests | 25-30% slower reaction time | Minimal to none |
| Next-day drowsiness | Common (37% of users report it) | Rare (under 5% report it) |
| Interaction with alcohol | Strongly increases risk | Minimal interaction |
| Occupational safety rating | High risk | Low risk |

Who’s Most at Risk?
It’s not just truck drivers. Pilots are banned from using first-generation antihistamines by the FAA. Why? They’re the most common drug found in the blood of pilots who died in crashes. Construction workers, factory operators, nurses on night shifts, warehouse staff, and even firefighters can be put at risk by these medications.
Older adults are especially vulnerable. The CDC says more than one in four adults over 65 fall each year. Sedating antihistamines increase that risk by causing dizziness, confusion, and poor balance. A 70-year-old warehouse worker taking Benadryl for allergies might not feel drunk-but their coordination is off enough to miss a step on a ladder.
And it’s not just accidents. Productivity takes a hit too. Workers on these drugs make more mistakes, take longer to complete tasks, and have higher error rates on memory and attention tests. One nurse working night shifts switched from diphenhydramine to loratadine and noticed immediate improvement: "I could focus better during procedures. I didn’t feel like I was moving through fog."
What Employers and Workers Need to Do
Most workplaces don’t have policies about antihistamines. That’s a problem. The National Safety Council found that only 41% of Fortune 500 companies include antihistamine guidance in their safety protocols as of 2023. That’s not enough.
Here’s what needs to change:
- Switch to non-sedating options. If you’re in a safety-sensitive job, use loratadine, fexofenadine, or bilastine. They work just as well for allergies without the brain fog.
- Don’t assume you’re fine. Even if you’ve taken Benadryl for years without feeling sleepy, your brain might still be impaired. Try a new antihistamine at home first. Wait 4-6 hours. Can you still tie your shoes? Recite your phone number backward? Drive around the block? If not, don’t take it before work.
- Time it right. If you must take a sedating antihistamine, take it at bedtime. But even then, wait at least 18-24 hours before operating machinery or driving. Some experts recommend 24 hours minimum for safety-sensitive roles.
- Read the label. FDA labels now require clearer warnings about driving and operating machinery. But many people skip them. If it says "may cause drowsiness," take it seriously-even if you think it doesn’t affect you.
- Train your team. Employers should include antihistamine risks in safety training. Make it part of your drug policy, just like alcohol or opioids.
What’s Changing? The Future of Antihistamine Safety
Regulators are catching up. In 2023, the FDA updated labeling rules to make warnings about occupational impairment more prominent. The European Medicines Agency already issued safety alerts for transport workers in 2019. NIOSH launched a new initiative in 2024 to create workplace antihistamine safety guidelines.
Market trends are shifting too. Second-generation antihistamines now make up 68% of the global market. Nurses are switching-73% of those surveyed use non-sedating options exclusively. Employers are starting to notice. In workplaces with safety-sensitive roles, the push is clear: stop using the old stuff.
The American College of Occupational and Environmental Medicine predicts that within the next five years, employers will require workers in safety-critical jobs to use only non-sedating antihistamines. That’s 23 million American workers who currently use sedating versions. Change is coming. The question is: will you be ready?
What to Do Today
If you take antihistamines and work in any job where focus, reaction time, or coordination matters, here’s your action plan:
- Check your medicine bottle. Is it diphenhydramine, chlorpheniramine, or hydroxyzine? If yes, stop using it for daytime allergy relief.
- Switch to loratadine, fexofenadine, or cetirizine. They’re available over the counter and cost about the same.
- Take your new medication at home for the first time. Test your alertness before going to work.
- Ask your pharmacist or doctor: "Is this safe for someone who drives or operates machinery?" Don’t assume they know.
- If you’re a manager or supervisor, review your workplace safety policy. Add antihistamines to your list of impairing substances.
There’s no shame in choosing a safer option. Allergies don’t have to cost you your safety-or someone else’s.
Can I still use Benadryl if I take it at night?
It’s risky. First-generation antihistamines like Benadryl can linger in your system for up to 30 hours. Even if you take it at bedtime, you may still be impaired the next day. Studies show 37% of users report next-day drowsiness. If you work in safety-sensitive roles-driving, operating machinery, or handling hazardous materials-wait at least 24 hours after your last dose before returning to duty.
Do all antihistamines make you drowsy?
No. Only first-generation antihistamines like diphenhydramine and chlorpheniramine are strongly linked to drowsiness. Second-generation options like loratadine (Claritin), fexofenadine (Allegra), and cetirizine (Zyrtec) are designed to avoid the brain and rarely cause sedation. About 78% of Allegra users report no drowsiness, compared to just 12% of Benadryl users.
Is it illegal to drive after taking an antihistamine?
It’s not specifically illegal to drive after taking an antihistamine-but it can be considered driving while impaired, which is illegal. Most U.S. states have laws that prohibit operating a vehicle under the influence of any substance that impairs your ability to drive safely. If you’re pulled over and fail a field sobriety test after taking Benadryl, you could be charged with DUI-even if you didn’t drink alcohol.
Why do doctors still prescribe sedating antihistamines?
They’re cheap, widely available, and effective for short-term relief. Many doctors assume patients will read the label and avoid using them during the day. But studies show most people don’t. In fact, a 2001 study found sedating antihistamines are still commonly prescribed despite known risks. The good news? More doctors are now switching to non-sedating alternatives, especially for patients in safety-sensitive jobs.
Can I mix antihistamines with alcohol or painkillers?
Never mix first-generation antihistamines with alcohol, opioids, benzodiazepines, or sleep aids. These combinations can multiply drowsiness and slow your breathing. Even small amounts of alcohol with Benadryl can make you as impaired as someone with a blood alcohol level of 0.08%. The FDA label on diphenhydramine explicitly warns against combining it with other CNS depressants.


Ben Jackson
October 28, 2025 AT 23:08Just had a safety meeting at the warehouse last week where they brought this up. Nobody knew how long Benadryl sticks around. We’ve got guys taking it for sinus stuff and then operating forklifts like it’s no big deal. I switched to Allegra six months ago-no more afternoon zoning out during inventory. Seriously, if your job involves moving stuff or people, don’t gamble with first-gen meds. The math doesn’t lie.
Meredith Poley
October 29, 2025 AT 05:56So let me get this straight: we’re having a national conversation about whether it’s safe to take allergy pills while driving, but we still let people drive with cracked windshields and bald tires? The real public health crisis is our refusal to regulate anything that doesn’t involve guns or weed.
Bhanu pratap
October 29, 2025 AT 11:13This is the kind of post that makes you stop and think. I’m from India, and here everyone just grabs Benadryl like candy when the pollen hits. My cousin, a delivery driver, was almost in an accident last spring-he blamed the heat. Turns out, it was the antihistamine. I showed him this article. He switched to Claritin yesterday. No more nightmares about his kid losing their dad because nobody told him the truth. Thanks for saying it loud.
Ikenga Uzoamaka
October 31, 2025 AT 03:33Are you kidding me?!?!? I’ve been taking diphenhydramine for 12 years, and I’ve never felt sleepy!!! I drive 80 miles to work every day, work a 12-hour shift in a factory, and then go to night school!!! You think I’m gonna stop because some ‘study’ says my brain is ‘impaired’??? I’m fine!!! You people need to stop scaremongering!!!
Adam Walter
November 1, 2025 AT 17:33Let’s be real-this isn’t just about antihistamines. It’s about how we’ve normalized chemical self-medication in America. We pop pills for everything: stress, sleep, allergies, focus-and then act shocked when we’re not fully present. I work ER nights. I’ve seen the aftermath: the guy who hit a tree because he took Benadryl for his sneezes, the nurse who missed a critical lab result because she was ‘just a little foggy.’ It’s not about being lazy. It’s about not knowing the cost. The second-gen options? They’re not ‘newfangled.’ They’re science. Use them.
Gurupriya Dutta
November 3, 2025 AT 09:50I’m a nurse, and I used to take Zyrtec at night because I thought it was ‘non-drowsy’-but I still felt off the next morning. I switched to fexofenadine and noticed the difference in my morning rounds immediately. I don’t miss doses anymore, and I feel like I’m actually present with my patients. It’s small, but it matters. I wish more people knew this.
Mathias Matengu Mabuta
November 3, 2025 AT 14:51While the data presented is statistically sound and methodologically rigorous, it is imperative to note that the generalization of impairment across occupational contexts is an oversimplification. The P-glycoprotein efflux mechanism, while well-documented in vitro, exhibits significant inter-individual variability due to polymorphisms in the ABCB1 gene. Furthermore, the cited 2013 driving simulator study employed a cohort of healthy young adults-demographics not representative of the aging workforce most vulnerable to sedative accumulation. The assertion that ‘second-generation antihistamines are safe’ is therefore an incomplete conclusion, and regulatory policy must account for pharmacogenomic heterogeneity. Additionally, the conflation of ‘drowsiness’ with ‘cognitive impairment’ remains a persistent epistemological flaw in public health messaging.
caroline howard
November 5, 2025 AT 04:53My boss just told me I can’t take Benadryl anymore. I cried. Not because I’m mad-because I realized I’ve been running on fumes for years. I thought I was ‘toughing it out.’ Turns out, I was just slow. I switched to Claritin. I didn’t even notice the change until I caught myself smiling at a coworker for no reason. Turns out, I’d forgotten what it felt like to be awake.
Michael Lynch
November 7, 2025 AT 04:29It’s funny how we treat our brains like they’re disposable. We’ll change the oil in our cars every 5,000 miles but take whatever pill feels good without asking how it affects the engine. Maybe the real question isn’t ‘which antihistamine?’ but ‘why do we keep pretending our bodies aren’t biological systems?’